Anthrax - PowerPoint PPT Presentation
1 / 67
Title:
Anthrax
Description:
Anthrax as a bioweapon. Aerosol method of delivery. Most likely method expected in BT attack ... Accidental release from anthrax drying plant. 79 human cases ... – PowerPoint PPT presentation
Number of Views:168
Avg rating:3.0/5.0
Title: Anthrax
1
Anthrax
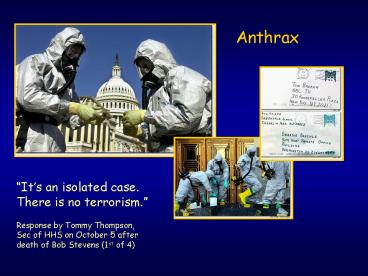
Its an isolated case. There is no
terrorism. Response by Tommy Thompson, Sec of
HHS on October 5 after death of Bob Stevens (1st
of 4)
2
Anthrax
- Caused by Bacillus anthracis
- Human zoonotic disease
- Spores found in soil worldwide
- Primarily disease of herbivorous animals
- Sheep, goats, cattle
- Many large documented epizootics
- Occasional human disease
- Epidemics have occurred but uncommon
- Rare in developed world
3
Anthrax as a bioweapon
- Many countries have weaponized anthrax
- Former bioweapon programs
- U.S.S.R.,U.S.,U.K., and Japan
- Recent bioweapon programs
- Iraq
- Attempted uses as bioterrorism agent
- WW I Germans inoculated Allied livestock
- WW II Alleged Japanese use on prisoners
4
Anthrax as a bioweapon
- Features of anthrax suitable as BT agent
- Fairly easy to obtain, produce and store
- Spores easily dispersed as aerosol
- Moderately infectious
- High mortality for inhalational (86-100)
5
Anthrax as a bioweapon
- Aerosol method of delivery
- Most likely method expected in BT attack
- Would cause primarily inhalational disease
- Spores reside on particles of 1-5 µm size
- Optimal size for deposition into alveoli
- Form of disease with highest mortality
- Would infect the largest number of people
6
Anthrax as a bioweapon
- Dispersed as powder
- Frequent letter hoaxes since 1997
- Recent letter deliveries
- Highest risk is for cutaneous
- Inhalational theoretically possible
- Particle size
- Likelihood of aerosolization
- GI theoretically possible
- Spores gt hands gt eating without handwashing
7
Anthrax as a bioweapon
- Sverdlovsk, Russia 1979
- Accidental release from anthrax drying plant
- 79 human cases
- All downwind of plant
- 68 deaths
- Some infected with multiples strains
8
Sverdlovsk Anthrax Incident
9
Dispersion of anthraxspores
10
Anthrax as a bioweapon
- Estimated effects of inhalational anthrax
- 100 kg spores released over city size of
Washington DC - 130,000 3 million deaths depending on weather
conditions - Economic impact
- 26.2 billion/100,000 exposed people
11
Anthrax Epidemiology
- Three forms of natural disease
- Inhalational
- Rare (lt5)
- Most likely encountered in bioterrorism event
- Cutaneous
- Most common (95)
- Direct contact of spores on skin
- Gastrointestinal
- Rare (lt5)
- Ingestion
12
Anthrax Epidemiology
- All ages and genders affected
- Occurs worldwide
- Endemic areas - Africa, Asia
- True incidence not known
- World
- 20,000-100,000 in 1958
- U.S.
- 235 total reported cases 1955-1994
- 18 cases inhalational since 1900, last one 1976
13
Anthrax Epidemiology
- Mortality
- Inhalational
- High even if treated (gt60)
- 100 if untreated or incomplete treatment
- Cutaneous
- lt5 (treated) 20 (untreated)
- GI approaches
- 25-60 if untreated
14
Anthrax Epidemiology
- Historical risk factors
- Agricultural
- Exposure to livestock
- Occupational
- Exposure to wool and hides
- Woolsorters disease inhalational anthrax
- Rarely laboratory-acquired
15
Anthrax Epidemiology
- Transmission
- No human-to-human
- Naturally occurring cases
- Skin exposure
- Ingestion
- Airborne
- Bioterrorism
- Aerosol (likely)
- Small volume powder (possible)
- Foodborne (unlikely)
16
Anthrax Epidemiology
- Transmission
- Inhalational
- Handling hides/skins of infected animals
- Microbiology laboratory
- Intentional aerosol release
- Small volume powdered form
- In letters, packages, etc
- Questionable risk, probably small
17
Anthrax Epidemiology
- Transmission
- Cutaneous
- Handling hides/skins of infected animals
- Bites from arthropods (very rare)
- Handling powdered form in letters, etc.
- Intentional aerosol release
- May see some cutaneous if large-scale
18
Anthrax Epidemiology
- Transmission
- Gastrointestinal
- Ingestion of meat from infected animal
- Ingestion of intentionally contaminated food
- Not likely in large scale
- Spores not as viable in large volumes of water
- Ingestion from powder-contaminated hands
- Inhalational of spores on particles gt5 ?m
- Land in oropharynx
19
Anthrax Microbiology
- Agent Bacillus anthracis
- Aerobic, Gram positive rod
- Long (1-10µm), thin (0.5-2.5µm)
- Forms inert spores when exposed to O2
- Infectious form, hardy
- Approx 1µm in size
- Vegetative bacillus state in vivo
- Result of spore germination
- Non-infectious, fragile
20
Anthrax Microbiology
- Environmental Survival
- Spores are hardy
- Resistant to drying, boiling lt10 minutes
- Survive for years in soil
- Still viable for decades in perma-frost
- Favorable soil factors for spore viability
- High moisture
- Organic content
- Alkaline pH
- High calcium concentration
21
Anthrax Pathogenesis
- Inhalational
- Spores on particles 1-5 ?m
- Inhaled and deposited into alveoli
- Estimated LD50 2500 55,000 spores
- Dose required for lethal infection in 50 exposed
- Contained in imperceptibly small volume
22
Anthrax Pathogenesis
- Inhalational
- Phagocytosed by alveolar macrophages
- Migration to mediastinal/hilar lymph nodes
- Germination into vegetative bacilli
- Triggered by nutrient-rich environment
- May be delayed up to 60 days
- Factors not completely understood
- Dose, host factors likely play a role
- Antibiotic exposure may contribute
- Delayed germination after antibiotic suppression
23
Anthrax Pathogenesis
- Inhalational
- Vegetative bacillus is the virulent phase
- Active toxin production
- Hemorrhagic necrotizing mediastinitis
- Hallmark of inhalational anthrax
- widened mediastinum on chest X-ray
- Does NOT cause pneumonia
- Followed by high-grade bacteremia
- Seeding of multiple organs, including meninges
24
Anthrax Pathogenesis
25
Anthrax Clinical
- Cutaneous
- by contact of infected animal carcasses or
contaminated wool, hides, fur - spores enter broken skin (cut, abrasion)
- common sites head, hands, forearm
- itching at site of entry
26
Anthrax Clinical
- Cutaneous
- papule formation becomes vesicle, then depressed,
black eschar (center necrotic area) with little
or no pain - local lymphadenopathy
- if untreated, can lead to septicemia, death (case
fatality ratio 5-20)
27
Anthrax Clinical
Cutaneous anthrax eschar (note central necrosis)
From CDC website www.bt.cdc.gov
28
Anthrax Clinical
- Inhalational
- Asymptomatic incubation period
- Duration 2-43 days, 10 days in Sverdlovsk
- Prodromal phase
- Correlates with germination, toxin production
- Nonspecific flu-like symptoms
- Fever, malaise, myalgias
- Dyspnea, nonproductive cough, mild chest
discomfort - Duration several hours to 3 days
- Can have transient resolution before next phase
29
Anthrax Clinical
- Inhalational
- Fulminant Phase
- Correlates with high-grade bacteremia/toxemia
- Critically Ill
- Fever, diaphoresis
- Respiratory distress/failure, cyanosis
- Septic shock, multiorgan failure, DIC
- 50 develop hemorrhagic meningitis
- Headache, meningismus, delirium, coma
- May be most prominent finding
- Usually progresses to death in lt36 hrs
- Mean time from symptom onset to death 3 days
30
Anthrax Clinical
- Inhalational
Characteristic mediastinal widening (arrows) From
JAMA 19992811735-1745
31
Anthrax Clinical
B. anthracis bacteria (arrows) in infected lung
tissue
32
Anthrax Clinical
Electron microscopy of B. anthracis bacteria
(arrow) filling capillary of animal with fatal
infection (X1250)
33
Anthrax Clinical
- Gastrointestinal
- Oropharyngeal
- Oral or esophageal ulcer
- Regional lymphadenopathy
- Edema, ascites
- Sepsis
- Abdominal
- Early symptoms - nausea, vomiting, malaise
- Late - hematochezia, acute abdomen, ascites
34
Anthrax Clinical
- Disease in animals
- peracute (apoplectic)
- mostly in cattle, sheep, goats
- subacute and acute
- common in cattle, horses and sheep
- fever (up to 107º F)
- hemorrhage from natural orifices
- edema
- excitement followed by depression
- respiratory distress
- uncoordination
- death
- Chronic
- generally in less susceptible animals such as
swine, but can be seen in cattle, horses, and dogs
35
Anthrax Diagnosis
- Early diagnosis is difficult
- Non specific symptoms
- Initially mild
- No readily available rapid specific tests
36
Anthrax Diagnosis
- Presumptive diagnosis
- History of possible exposure
- Typical signs symptoms
- Rapidly progressing nonspecific illness
- Widened mediastinum on CXR
- Large Gram bacilli from specimens
- Can be seen on Gram stain if hi-grade bacteremia
- Appropriate colonial morphology
- Necrotizing mediastinitis, meningitis at autopsy
37
Anthrax Diagnosis
- Definitive diagnosis
- Direct culture on standard blood agar
- Gold standard, widely available
- Alert lab to work up Gram bacilli if found
- 6-24 hours to grow
- Sensitivity depends on severity, prior antibiotic
- Blood, fluid from skin lesions, pleural fluid,
CSF, ascites - Sputum unlikely to be helpful (not a pneumonia)
- Very high specificity if non-motile,
non-hemolytic - Requires biochemical tests for gt99 confirmation
- Available at Reference laboratories
38
Anthrax Diagnosis
- Definitive diagnosis
- Rapid confirmatory tests
- Role is to confirm if cultures are negative
- Polymerase Chain Reaction (PCR)
- Hi sensitivity and specificity
- Detects DNA
- Viable bacteria/spores not required
- Immunohistochemical stains
- Most clinical specimens can be used
39
Anthrax Diagnosis
- Testing for exposure
- Nasal swabs
- Can detect spores prior to illness
- Currently used only as epidemiologic tool
- Decision for PEP based on exposure risk
- May be useful for antibiotic sensitivity in
exposed - Culture on standard media
- Swabs of nares and facial skin
- Serology
- May be useful from epidemiologic standpoint
40
Anthrax Diagnosis
- Environmental samples
- Suspicious powders
- Must be sent to reference laboratories as part of
epidemiologic/criminal investigation - Assessed using cultures, stains, PCR
- Air sampling
- First responders
- Handheld immunoassays
- Not validated
- Useful for detecting massive contamination
41
Anthrax Diagnosis
42
Anthrax Diagnosis
Direct smear from blood stained with p-c-m
blue (From http//gsbs.utmb.edu/microbook/ch015.ht
m)
43
Anthrax Diagnosis
Source http//www.geocities.com/vadivale
44
Anthrax Treatment
- Immediately treat presumptive cases
- Prior to confirmation
- Rapid antibiotics may improve survival
- Differentiate cases vs exposed
- Cases
- Potentially exposed with any signs/symptoms
- Exposed
- Potentially exposed but asymptomatic
- Provide Post-Exposure Prophylaxis
45
Anthrax Treatment
- Antibiotic selection
- Naturally occurring strains
- Rare penicillin resistance
- Penicillins, aminoglycosides, tetracyclines,
erythromycin, chloramphenicol effective - Ciprofloxacin very effective (animal studies)
- Other fluoroquinolones probably effective
- Engineered strains
- Known penicillin, tetracycline resistance
- Highly resistant strains mortality of untreated
46
Anthrax Treatment
- Empiric Therapy
- Until susceptibility patterns known
- Adults
- Ciprofloxacin 400 mg IV q12hrs
- OR
- Doxycycline 100mg IV q12hrs
- AND
- One or two other antibiotics
- (for inhalational)
47
Anthrax Treatment
- Empiric Therapy
- Children
- Ciprofloxacin 10-15 mg/kg/d IV q12, max 1 g/d
- OR
- Doxycycline 2.2 mg/kg IV q12
- (adult dosage if gt8 yo and gt45 kg)
- Add one or two antibiotics for inhalational
- Weigh risks (arthropathy, dental enamel)
48
Anthrax Treatment
- Empiric therapy
- Pregnant women
- Same as other adults
- Weigh small risks (fetal arthropathy) vs benefit
- Immunosuppressed
- same as other adults
49
Anthrax Treatment
- Antibiotic therapy
- Duration
- 60 days
- Risk of delayed spore germination
- Vaccine availability
- Could reduce to 30-45 days therapy
- Stop antibiotics after 3rd vaccine dose
- Switch to oral
- Clinical improvement
- Patient able to tolerate oral medications
50
Postexposure Prophylaxis
- Who should receive PEP?
- Anyone exposed to anthrax
- Not for contacts of cases, unless also exposed
- What?
- Empiric antibiotic therapy
- Treat ASAP
- Prompt therapy can improve survival
- Continue for 60 days
- 30-45 days if vaccine administered
- Vaccination
51
Anthrax Prevention
- Vaccine
- Anthrax Vaccine Adsorpbed (AVA)
- Supply
- Limited, controlled by CDC
- Production problems
- Single producer Bioport, Michigan
- Failed FDA standards
- None produced since 1998
52
Anthrax Prevention
- Vaccine
- Inactivated, cell-free filtrate
- Adsorbed onto Al(OH)3
- Protective Antigen
- Immunogenic component
- Necessary but not sufficient
- Administration
- Dose schedule
- 0, 2 4 wks 6, 12 18 months initial series
- Annual booster
- 0.5 ml SQ
53
Anthrax Prevention
- Vaccine Efficacy
- gt95 protection vs. aerosol in animal models
- gt90 vs. cutaneous in humans
- Older vaccine that was less immunogenic
- Protection vs inhalational but too few cases to
confirm - Safety Adverse Effects
- gt1.6 million doses given to military by 4/2000
- No deaths
- lt10 moderate/severe local reactions
- Erythema, edema
- lt1 systemic reactions
- Fever, malaise
54
Infection Control
- No person to person transmission
- Standard Precautions
- Laboratory safety
- Biosafety Level (BSL) 2 Precautions
55
Infection Control
- No person to person transmission
- Standard Precautions
- Laboratory safety
- Biosafety Level (BSL) 2 Precautions
56
Laboratory Response NetworkFor Bioterrorism
- Highest level characterization (Federal)
- Molecular assays
- reference capacity
- Limited confirmation
- and transport
- Rule out and forward
- organisms
- Level D Lab
- BSL-4
- Level C Lab
- BSL-3
- Level B Lab
- BSL-2 BLS-3 safety practices
- Level A Lab
- Class 2 biosafety cabinet
57
Decontamination
- Highest risk of infection at initial release
- Duration of aerosol viability
- Several hours to one day under optimal conditions
- Covert aerosol long dispersed by recognition 1st
case - Risk of secondary aerosolization is low
- Heavily contaminated small areas
- May benefit from decontamination
- Decontamination may not be feasible for large
areas
58
Decontamination
- Skin, clothing
- Thorough washing with soap and water
- Avoid bleach on skin
- Instruments for invasive procedures
- Sterilize, e.g. 5 hypochlorite solution
- Sporicidal agents
- Sodium or calcium hypochlorite (bleach)
59
Decontamination
- Suspicious letters/packages
- Do not open or shake
- Place in plastic bag or leakproof container
- If visibly contaminated or container unavailable
- Gently cover paper, clothing, box, trash can
- Leave room/area, isolate room from others
- Thoroughly wash hands with soap and water
- Report to local security / law enforcement
- List all persons in vicinity
60
Decontamination
- Opened envelope with suspicious substance
- Gently cover, avoid all contact
- Leave room and isolate from others
- Thoroughly wash hands with soap and water
- Notify local security / law enforcement
- Carefully remove outer clothing, put in plastic
- Shower with soap and water
- List all persons in area
61
Current Outbreak Investigation
- Case definitions
- Confirmed case
- Clinically compatible syndrome
- culture or 2 non-culture diagnostics
- Presumptive case
- Clinically compatible syndrome
- 1 non-culture diagnostic or confirmed exposure
- Exposures
- Confirmed exposure
- May be aided by nasal swab cultures, serology
- Asymptomatic
62
Current Outbreak Investigation
63
Current Outbreak Investigation
NY letters
DC letter
Number of cases (all)
October
September
Postmarked data of known contaminated letter
MMWR 200150(43)941-948
64
How Can I Protect Myself from Mail Contaminated
with Anthrax?
- Do not shake or empty the contents of a
suspicious package or envelope. - Do not carry the package or envelope, show it to
others, or allow others to examine it. - Put the package or envelope on a stable surface
do not sniff, touch, taste, or look closely at it
or any contents that may have spilled. - Alert others in the area about the suspicious
package or envelope. Leave the area, close any
doors, and take actions to prevent others from
entering the area. If possible, shut off the
ventilation system.
65
How Can I Protect Myself from Mail Contaminated
with Anthrax?
- Wash hands with soap and water to prevent
spreading potentially infectious material to face
or skin. Seek additional instructions for exposed
or potentially exposed persons. - If at work, notify a supervisor, a security
officer, or a law enforcement official. If at
home, contact the local law enforcement agency. - If possible, create a list of persons who were in
the room or area when this suspicious letter or
package was recognized and a list of persons who
also may have handled this package or letter.
Give the list to both the local public health
authorities and law enforcement officials.
66
Pervasive nature of current situation
67
(No Transcript)