HIV PowerPoint PPT Presentation
1 / 1
Title: HIV
1
HIV Delivery Clinical Characteristics
Outcomes
Shalika Basnayake Katugaha, MD1 Alison Vogell,
MD2 Kathryn Smith, MD3 Geeta Karnik, MD4
Hilda Audardottir-Goulay5 Princy Kumar, MD6
Joseph Timpone, MD7, Mary Young, MD8
1Division of Infectious Disease, Georgetown
University Hospital 2Georgetown University
Hospital 3Department of Obstetrics Gynecology,
Georgetown University Hospital 4Department of
Medicine, Georgetown University Hospital
5Division of Infectious Disease, Georgetown
University Hospital 6Division of Infectious
Disease, Georgetown University Hospital
7Division of Infectious Disease, Georgetown
University Hospital 8Division of Infectious
Disease, Georgetown University Hospital
Georgetown University
Introduction
Methods
Results
Obstetrical Complications
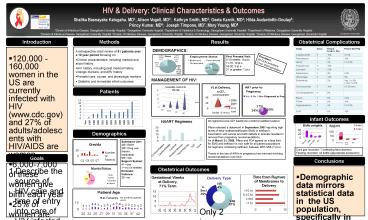
- A retrospective chart review of 51 patients over
a 10 year period focusing on - Clinical characteristics, including medical and
social history - HIV history, including past medical history,
virologic markers, and ARV history - Prenatal care, course, and physiologic markers
- Obstetric and immediate infant outcomes
- 120,000 -160,000 women in the US are currently
infected with HIV (www.cdc.gov) and 27 of
adults/adolescents with HIV/AIDS are women - 6,000-7,000 of these women give birth each year
- 25 of women are unaware of their HIV status
- In the era of HAART, perinatal HIV infection is
less than 2 in the United States - Public Health Service Task Force Recommendations,
April 29, 2009 - Combination antepartum antiretroviral drug
regimens are more effective than single-drug
regimens - Inclusion of AZT is recommended in pregnancy
regimens - Longer duration of antepartum prophylaxis is
more effective than shorter therefore, for women
who do not require immediate initiation of
therapy for their own health, prophylaxis should
be started by 28 weeks gestation - Breastfeeding is not recommended for
HIV-infected women in the US - No indication for C-section for patients with
viral loadlt1000
DEMOGRAPHICS
First Prenatal Visit 5-10 weeks 18 pt.s 11-15
10 pt.s 16-20 3 pt.s 21 or greater 7 pt.s
Providers 34 GUH providers 2 non GUH providers
MANAGEMENT OF HIV
Patients
Infant Outcomes
All regimens have AZT backbone (combivirazt/lamiv
udine) Pfizer released a statement in September
2007 reporting high levels of ethyl
methanesulfonate (EMS) in nelfinavir Association
with cancer and birth defects in animals resulted
in removal from pregnancy recommendations As of
March 31, 2008, Pfizer and FDA agreed on a final
limit for EMS and nelfinavir is now safe for all
patient populations No regimens containing
nelfinavir between 9/07-3/08 (7 pt.s) Trends in
the use of ARVs in pregnancy has mirrored
evolving recommendations over time
Demographics
Substance Use 2/51 EtOH 2/51 Drug use (heroin,
marijuana) 5/51 Tob Support System 41yes 1no
(in shelter) Domestic Violence 32no
Cord gas recorded 7 (reflecting fetal
distress) Feeding recorded 44 bottle
(appropriate precaution)
Goals
Conclusions
- Describe the source of HIV care and time of entry
into care of HIV infected women at an urban
teaching hospital - To assess the clinical characteristics and
demographics of HIV pregnant women over an
evolving time period - In the era of HAART, to describe the use of ARVs
in the HIV infected pregnant population to assess
immunologic and virologic response - To assess the obstetrical and infant outcomes in
HIV infected pregnant women
Obstetrical Outcomes
- Demographic data mirrors statistical data in the
US population, specifically in Washington, DC - of African American women with HIV
- of women unaware of diagnosis at preg
- Data reflects that in the era of HAART, most
women do become undetectable by delivery - In spite of the overall number of
immunosuppressed women - Trends in the use of HAART in pregnancy reflect
evolving recommendations over time - Obstetrical outcomes suggest that women with HIV
have a very similar experience at delivery as the
general population - Immediate infant outcomes reflect no adverse
events
Only 2 in series meet ID criteria for C-section