Case report PowerPoint PPT Presentation
1 / 62
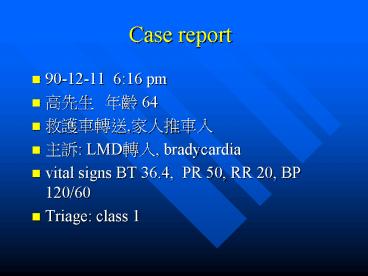
Title: Case report
1
Case report
- 90-12-11 616 pm
- ??? ?? 64
- ?????,?????
- ?? LMD??, bradycardia
- vital signs BT 36.4, PR 50, RR 20, BP 120/60
- Triage class 1
2
- LMD Transfer note
- A middle aged male patient suffered from chest
distress with SOB, and he was sent to our H. At
ER complete ECG revealed mild ST-T elevation in
II and aVF, and bradycardia was also noted and he
received NTG 1 sl st and nasal O2 therapy, but
s/s persisted - R/O inf. MI Thanks for your attention
3
- Chief Complaint OPD ?, R/O AMI
- Present Illness
- Chest pain onset at 500 pm
- No radiate to back
- Radiate to neck
- Past personal and medical history
- ??????
- Smoking drinking
- HTN(-)
4
PE
- vital signs BT 36.4, PR 50, RR 20, BP 120/60
- Consciousness clear
- HEENT and neck No JVD
- Chest regular heart beat, bradycardia
- Abdomen Soft
- Pelvix Stable
- Ext symmetric 4 limbs pulse
- NE normal
- Impression???
5
Impression
- R/O AMI
6
Order sheet
- CBC/DC/PLT
- PT,aPTT
- ??
- N/S KVO
- NTG spray sl 2
- Morphine 3 mg iv st
- millisrol 3 cc/hr
- on monitor
7
Order sheet
- Troponin T
- portable CXR
- Rt side ECG
- ECG
8
ECG bradycardia
9
710 pm order
- Impression bradycardia, r/o hyperkalemia
- Calcium gluconate 1 amp iv st
10
750 pm Lab Data
- Glu110, BUN15, Cr1.1, Na146, K4.1
- CPK 107, CKMB 13
- Troponin Ilt 0.5
11
750 pm progress note
- S still chest pain
- O nausea(), Vomiting() 2 times
- pain will increase by inspiration or swallowing
- radiate to neck
- Not chest tightness
- Lab data K4.1 Tro.Ilt0.5 CKMB13 CK107
- A chest pain and bradycardia, cause ?
- P
- f/u cardiac enzyme
- check 4 limbs BP
12
Order sheet 810 pm
- F/U Troponin I, CPK, CKMB at 830 pm
- check 4 limbs BP st
- F/U ECG at 830 pm
13
845 ECG
14
840 pm
- 4 limbs BP
- RU 89/72 mmHg, LU 117/68 mmHg
- RL 151/81 mmHg, LL 141/78 mmHg
15
900 pm Progress note
- Rt upper limb cold, weak pulse
- Still chest pain
- CXR boulderline widening mediastinum
- R/O aortic disection
- arrange chest CT
16
919 pm Lab Data
- CPK 100
- CKMB 10
- Troponin I lt 0.5
17
920 pm progress note
- S chest severe pain
- O consciousness slear
- BP 100/60, PR 50 RR 16/min
- Neck supple
- Heart RHB with murmur
- lung clear
- Abdomen soft.normal active bowel sounds
18
920 pm progress note
- Ext
- muscle power 4 symmetric,
- Pulse RU limb , LU limb , RL and LL limb
- Aortic CT definite dissection in ascending aorta
- P
- control BP and PR
- consult CVS
19
1030 pm CVS note
- Aortic dissection, type A
- surgical repair is indicated
- admit to SICU for BP control and preop preparation
20
Aortic Dissection
- Manifestation
- Pain gt 90
- vasovagal symptoms
- Syncope 5
- neurologic deficit 20
21
Pain
- the most common complaint (gt 90 of cases)
- In almost all cases in which pain is not present,
the patient either is unconscious or has a
neurologic deficit that impairs pain perception. - tearing, ripping, and knifelike, but
may be characterized by different patients in
many different ways. - Typically the pain occurs abruptly and is most
severe at onset.
22
- The location of the pain
- Anterior chest pain -- dissection of the
ascending aorta - neck and jaw -- dissection of the aortic arch,
- in the interscapular area --descending thoracic
aorta - in the lumbar area or abdomen-- involvement below
the diaphragm - migration -- propagation of the dissection
- has very high diagnostic accuracy for aortic
dissection. - In one study, 71 of patients with aortic
dissection had migration of pain.
23
- Aortic dissection accompanied by vasovagal
symptoms - diaphoresis, nausea, vomiting, light-headedness,
and severe apprehension. - Syncope
- early course of aortic dissection, about 5 of
cases. - most associated with ascending aorta dissection
- dissection into the pericardium?pericardial
tamponade - Other causes of syncope secondary to aortic
dissection are hypovolemia, excessive vagal tone,
and cardiac conduction abnormalities.
24
- In approximately 20 of patients, neurologic
deficit is the presenting manifestation of aortic
dissection. - The neurologic presentations are CVA, spinal cord
ischemia, and peripheral nerve ischemia
25
Physical Examination.
- Appearance very apprehensive
- Tachycardia and signs of inadequate end-organ
perfusion may be present even in the face of an
elevated blood pressure. - e.g., clammy skin, altered mental status, delayed
capillary refill - chronic hypertension gt 75 of patients
- may be exacerbated by a catecholamine release
related to the acute event
26
- Severe hypertension refractory to medical therapy
- may occur if the dissection involvesthe renal
arteries with subsequent renin release - hypotension
- dissection has progressed back into the
pericardium with resulting pericardial tamponade - hypovolemia occurred from rupture along the aorta
- pseudohypotension
- the blood pressure in the arms is low or
unobtainable and the central arterial pressure is
normal orhigh. - results from the interruption of blood flow to
the subclavian arteries
27
Pulse deficits and discrepancies in blood
pressure between limbs
- Pulse deficits(a unilaterally weakened or absent
pulse) in almost 50 of patients with proximal
dissections - Usually in the upper extremities
- mechanisms
- An intimal flap cover the true lumen of a branch
vessel - dissecting hematoma compress an adjacent true
lumen. - Careful documentation of pulses and frequent
reexamination are important because pulse
deficits are commonly transient
28
Acute aortic regurgitation
- This is identified clinically by
- Hypotension
- fulminant pulmonary edema
- aortic diastolic murmur (musical, vibrating
quality with variable intensity) - widened mediastinum on CXR
- Aortic regurgitation in 50 of type A
dissections - Rapid surgical correction affords the only chance
for survival
29
- Hemorrhage into the pericardium or tamponade
??????? - Pericardial friction rub
- Jugular venous distension
- Pulsus paradoxus
- Muffled heart sounds
- Tachycardia
- Hypotension
30
Neurologic findings
- most common altered sensorium
- The most common focal neurologic abnormalities
- Hemiplegia
- Hemianesthesia
- Gaze preference to the affected side
- Ischemic paraparesis
- occurs in approximately 4 of dissections
- result of interruption of blood flow in the
intercostal, lumbar, and anterior spinal
arteries. - Ischemic peripheral neuropathy
- may follow obstruction of the vessels that supply
the upper and lower extremities
31
Uncommon clinical manifestations
- Hemoptysis
- a rare finding in aortic dissection and usually
is caused by rupture of the aorta into lung
tissue or by dissection of bronchial arteries - Hoarseness
- from vocal cord paralysis may be caused by
compression of the recurrent laryngeal nerve by
the expanding dissecting hematoma - Horners syndrome
- may result from compression of the superior
cervical sympathetic ganglion by the dissected
aorta. - Superior vena cava syndrome
32
- Hematemesis
- Rupture of the aorta into the esophagus
- Bronchospasm
- Bronchial or tracheal compression
- Mesenteric infarction and myocardial infarction
(MI) unusual - Rarely, aortic dissection may present as a fever
of unknown origin
33
Ancillary Evaluation
- Routine Laboratory Tests.
- of little value.
- Serial analysis of cardiac enzymes is usually
negative. - Microscopic hematuria may occur where the renal
artery is involved
34
ECG
- EKG
- Commonly shows LVH reflecting long-standing
hypertension - Useful in excluding MI however, 10 to 40 of
patients with aortic dissection may have EKG
abnormalities suggesting ischemia or infarction - Acute MI
- Proximal dissection that involves a coronary
artery - Heart block
- retrograde dissection into the interatrial septum
with compression of the AV node
35
Chest X-Ray
- Routine chest x-ray studies will be abnormal in
80 to 90 of cases. - mediastinal widening gt75 of cases.
- The calcium sign uncommon but highly specific
- the calcium deposit separated from the outermost
portion of the aorta gt 5 mm - Double-density appearance of the aorta
- suggesting true and false channels
36
- localized bulge along a normally smooth aortic
contour - disparity in the caliber between the descending
and ascending aorta - Displacement of the trachea or nasogastric tube
to the right by the dissection - Previous CXR very useful for comparison
- Pleural effusions are common and usually occur on
the left side - small effusion periaortic inflammation
- a large effusion leaking or rupture of the
dissection into the pleural space? Thoracentesis
37
Echocardiography
- Until recently, echocardiography has not been a
useful tool in the detection and delineation of
aortic dissection - M-mode and 2-D ultrasound through a transthoracic
approach have a sensitivity and specificity that
is unacceptably low, ranging from 77 to 80 and
93 to 96, respectively, giving a predictive
value that results in too many false-negative
tests - The transthoracic approach is hindered by
overlying sternum, ribs, and lungs
38
Transesophageal Echocardiography
- Dramatically improved the quality of
echocardiography in the diagnosis of aortic
dissection - This modality has been shown to be 97 to 100
sensitive and 90 to 100 specific - There can be some difficulty in evaluating the
ascending aorta and proximal arch because of the
interposition of the air-filled trachea and left
main bronchus, but this problem has been largely
overcome by the use of the newer biplane probes.
39
TEE
- Multiplane (or omniplane) probes may be of still
greater usefulness because they allow additional
views of cardiovascular structures in oblique
planes - Transesophageal echocardiography (TEE) is quick
and can be easily performed at the bedside in the
ED. - Few serious side effects or contraindications
- Requires no radiation or contrast injection.
40
TEE
- TEE is excellent at detecting pericardial
effusion and compares favorably with other
modalities in evaluating aortic regurgitation,
flow in the proximal coronary arteries, the
intimal flap, and site of entry. - For these reasons, TEE has become the primary
diagnostic method for detecting aortic dissection
in many institutions
41
CT
- The rates of both false-positive and
false-negative diagnoses of aortic dissection
appear to be less than 5. - Signs on the CT scan that are particularly
suggestive of aortic dissection include
dilatation of the aorta, identification of an
intimal flap, differential rates of flow in true
and false channels, and the clear demonstration
of both the false and true lumina.
42
Limitations of the CT scan
- It does not provide information about the
presence of aortic regurgitation, which is
important in determining appropriate therapy - Fails to provide reliable information about the
relationship of the dissection to the major
arterial branches of the aorta - Some patients have serious adverse reactions to
the administration of IV contrast material - A CT scan is time consuming and requires the
patient to be outside of the ED or intensive care
unit
43
Aortography
- In most institutions, aortography remains the
standard imaging modality for detection of aortic
dissection against which all other modalities are
measured - In skilled hands, this procedure can be performed
with low morbidity and mortality and with high
diagnostic accuracy
44
Aortography
- Filling of a false channel
- Channels with or without an intervening intimal
flap - Distortion of the true lumen by either a patent
or thrombosed false lumen - Thickening of the aortic wall by more than 5 to 6
mm caused by a thrombosed false lumen - Displaced intimal calcification
45
Aortography
- Misdiagnoses occur in one of several situations
- Thrombosis of the false channel may prevent
visualization of either the intimal flap or a
double lumen. - The true and false lumina may opacify
simultaneously and, therefore, may not be clearly
delineated from one another. - The intimal flap may not be visualized when it is
located in a plane tangential to the x-ray beam
46
The disadvantages of aortography
- invasive techniques, requires that a catheter be
inserted into a potentially abnormal aorta. - It is also the most expensive of the modalities
available. - Specialized personnel are required, and the
patient must be removed from the ED. - Other disadvantages are the risks of IV contrast
material and inadequate detection of pleural leak
47
Aortography
- Despite these limitations, aortography remains an
informative procedure to diagnose aortic
dissection. - It is a sensitive test for detecting aortic
dissection and very accurate for determining the
site of the intimal tear and the extent of the
dissection - Aortic regurgitation is easily demonstrated with
aortography, and it is the only procedure that
demonstrates the extent and location of
dissection into aortic side branches
48
CT versus Aortography
- The CT scan has greater contrast resolution and
detects small or delayed differences in the
opacification of true and false channels. - A CT scan may be able to detect a thrombosed
false lumen despite nonopacification, whereas
aortography cannot. - The axial scanning plane in a CT scan is
perpendicular to the intimal flap so that the
detection of the intimal flap is easier. - Does not require arterial catheterization, and
may reveal other abnormalities that explain the
patients clinical presentation
49
MRI
- For the evaluation of the stable patient with
suspected aortic dissection - Useful in
- the evaluation of chronic aortic dissection,
- in the follow-up of postoperative patients
- for monitoring nonoperative patients for
progression of the dissection
50
TREATMENT
51
Treatment at Emergency Department
- All patients suspected of having an acute aortic
dissection should receive careful monitoring of
cardiac rhythm, blood pressure, and urine output - The objectives of early management are to
eliminate the forces favoring progression of the
dissection by maintaining systolic blood pressure
between 100 and 120 mm Hg (or the lowest level
commensurate with vital organ perfusion) and by
reducing the force of cardiac contraction and the
rate of rise of the arterial pulse (dP/dT).
52
- Narcotics should be administered in adequate
amounts for pain control - Therapy should begin immediately to attain these
goals while other diagnostic tests are performed - The early hours are a critical period
- The mortality in the first 24 to 48 hours of
aortic dissection is between 1 and 2 per hour. - Those patients presenting with hypotension
secondary to aortic rupture or pericardial
tamponade should be resuscitated with IV fluids
and blood transfusions - More typically, the patient will be hypertensive
53
Sodium nitroprusside
- Prompt reduction of the blood pressure can be
accomplished with sodium nitroprusside - 50 to 100 mg are mixed in 500 ml of D5W and
initially infused at a rate of 0.5 to 3 mg/kg/min - The rate is adjusted to achieve the desired blood
pressure - The solution is light sensitive, and the bottle
and tubing containing the mixture should be
wrapped in aluminum foil
54
Sodium nitroprusside
- Because sodium nitroprusside increases the heart
rate and may also increase the dP/dT,
administration of this drug alone may worsen the
dissection - A b-adrenergic blocker must be used in
conjunction with sodium nitroprusside to lower
the dP/dT - Propranolol
- more selective b-blocking agent such as
metoprolol. - Esmolol short-acting (continuous infusion)
55
- Trimethaphan camsylate
- effective in the initial treatment of acute
aortic dissection - It is generally used as a single agent and is the
preferred drug in a patient who has a
contraindication to b-blockers - IV labetalol
- This drug has both a- and b-blockade properties
- May be used as a single agent for the management
of aortic dissection
56
Definitive Therapy
- Type A acute aortic dissections require surgical
treatment. - The aortic segment containing the original
intimal tear is resected when possible, with
graft replacement of the ascending aorta to
redirect blood into the true lumen. - An operative mortality rate of 7 has recently
been reported - If aortic insufficiency is present, it can be
corrected through aortic valve resuspension or
replacement
57
- The only contraindication to immediate surgical
repair of a type A dissection is the simultaneous
occurrence of a progressing stroke.
58
Type B acute aortic dissections
- Definitive treatment is less clear
- Generally, these patients tend to be worse
surgical risks - The hospital mortality in patients treated
without surgery who have acute type B dissections
is 15 to 20, and that is comparable to or
better than the mortality rate with surgery in
most institutions, although the mortality rate in
surgery for type B dissections appears to be
decreasing
59
Uncomplicated distal dissections
- Patients who present with chronic aortic
dissection have already survived their period of
greatest mortality risk and are usually treated
by blood pressure control unless complications
mandate surgery - Treated with blood pressure control
- Surgery has been reserved for those patients who
have persistent pain, uncontrolled hypertension,
occlusion of a major arterial trunk, frank aortic
leaking or rupture, or development of a localized
aneurysm
60
- However, as surgical management for these
patients improves, medical therapy may be
replaced by operative treatment as the preferred
definitive approach - All patients who have sustained and survived an
aortic dissection, regardless of the type of
definitive therapy used, require careful
long-term management - Major complications that may occur with time are
redissection, the development of a localized
aneurysm, and progressive aortic insufficiency
61
- Control of blood pressure is the cornerstone of
therapy - b-Blocking agents are the most commonly used oral
antihypertensive drugs in the treatment of these
patients - other agents, such as thiazide diuretics, calcium
channel blockers, and angiotensin-converting
enzyme inhibitors, may need to be added.
62
Follow-up visits
- Blood pressure monitoring
- Detecting signs of recurrence or progression of
disease - Chest pain
- Signs of congestive heart failure
- Presence of aortic insufficiency
- Mediastinal size can be followed by chest x-ray
studies. - Periodically these patients should undergo either
a CT scan or MRI scan to determine the status of
the aorta