Case Study - PowerPoint PPT Presentation
1 / 39
Title:
Case Study
Description:
Baby at 12 hours of life had worsening resp. ... Maintenance fluids have been started, Amp/Gent have been given. ... Pulmonary Atresia, tricuspid atresia, Tet. ... – PowerPoint PPT presentation
Number of Views:40
Avg rating:3.0/5.0
Title: Case Study
1
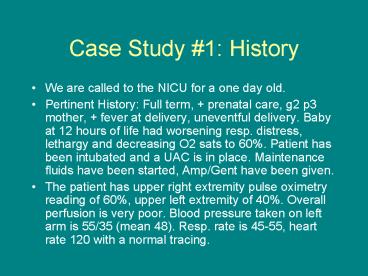
Case Study 1 History
- We are called to the NICU for a one day old.
- Pertinent History Full term, prenatal care, g2
p3 mother, fever at delivery, uneventful
delivery. Baby at 12 hours of life had worsening
resp. distress, lethargy and decreasing O2 sats
to 60. Patient has been intubated and a UAC is
in place. Maintenance fluids have been started,
Amp/Gent have been given. - The patient has upper right extremity pulse
oximetry reading of 60, upper left extremity of
40. Overall perfusion is very poor. Blood
pressure taken on left arm is 55/35 (mean 48).
Resp. rate is 45-55, heart rate 120 with a normal
tracing.
2
Case Study 1 Physical Exam
- The patients exam as reported over the phone is
significant for - Obtundation with mild movement, resp. failure,
femoral pulses, pupils 3mm bilat. Reactive,
fontanel wnl, abd. Wnl, loud systolic murmur at
LSB.
3
Case Study 1 Data
- CXR reveals large heart. No pulm.
consolidation,effusion, diaphragmatic hernia. - Electrolytes WNL
- WBC 12.5, Hct 45. Nl. Differential.
- ABG 6.8/35/45/-25
4
Case Study 1BEFORE you leave
- What are the most likely diagnosis?
- Thinking of the potential diagnosis allows
instructions to be given to the referring
hospital that may make a difference in the childs
condition while the team is en route. Always
think through the diagnosis. Your conclusion may
be different than the referring hospitals and
therapies may also differ. Discuss your concerns
with the attending in the PICU or NICU.
5
Case Study 1 Diff. Dx.
- Sepsis. Always a consideration in the sick
newborn. It can be a concomitant diagnosis. - The mother had a fever during delivery. GBS
status and other prenatal labs are unknown. - Broad spectrum antibiotics (Amp/Cefotaxime)
should be started.
6
Case Study 1 Diff. Dx.
- Congenital Heart Disease
- The presence of a murmur, hypoxia, resp. distress
is suspicious for CHD. - No Echo is available.
- Differential hypoxia suggest Aortic Coarctation
or other ductal dependent malformations.
7
Differential Diagnosis.
- Pulmonary Hypertension
- Hypoxia, resp failure, acidosis, hypotension.
- If there is a large PDA and small foramen ovale
(ie small amount of mixing) there could also be a
pre and post ductal gradient.
8
Case Study1 Diff. Dx.
- Respiratory etiologies Pneumonia, pulmonary
malformation, airway malformation, AVM
(pulmonary, cerebral, intrabdominal). - Inborn error of metabolism
9
Case Study 1 Before leaving
- The most likely diagnosis are sepsis vs.
co-arctation. - Recommend start PGE-1. Do not accept it if told
they will wait until the team arrives. All
hospitals have PGE-1 and can start the drip. If a
patient is not intubated impart that apnea and
hypotension are common effects of PGE-1 so they
can prepare for them. - Infant is severely acidotic. Recommend
NaBicarbonate bolus and drip if needed
10
Case Study 1 Arrival
- Upon arrival the patient is on the ventilator
pre-ductal pulse ox is 65, post ductal pulse ox
is 45-50. Patients heart rate is 60bpm, on
mechanical vent 25/4 rate of 30, 100 FiO2. BP in
right arm is 55/35. Perfusion is very poor baby
is cyanotic. - Your first move?
11
Case Study 1 Arrival
- BEGIN CPR. Patients heart rate is 60.
- .01 of 1/10000 Epi per UAC line.
- Take patient OFF vent and hand bag. The vent
setting may be inadequate. Assess if tube is in
correct place and functioning (SEE Xray
personally. NEVER take report unless there is no
alternative. Be polite but insistent (I usually
say its just my habit).
12
Arrival
- Patient responds to Epi. HR 124 with normal
tracing. - Perfusion remains poor.
- Your exam reveals infant moves with stimulation,
extremely poor perfusion, lung sounds clear
equal, equal nl femoral pulses, loud systolic
murmur. - You notice the pulse oximetry readings show equal
readings in the 65-70s at times and a pre and
post ductal readings other times.
13
Interventions
- Identify the problem list and attack it in order
of ABCs WHILE considering the diagnosis and
other potential diagnosis. Think through the
other differential possibilities when making
interventions to evaluate if your intervention
would be contraindicated with an alternative dx.
For example sepsis requires large amounts of
fluid while the same amount of fluid would worsen
a congenital heart malformation with failure.
14
Interventions
- Co-arctation remains the leading diagnosis
however a variety of congenital heart defects can
give the same clinical picture. The key is that
they may also be ductal dependant - Pulmonary Atresia, tricuspid atresia, Tet. Of
Fallot, interrupted aortic arch, transposition
of the great vessels (with or without intact
septum)
15
PGE-1
- Before starting be prepared for the two major
side effects - Apnea- prophylactic intubation if needed.
- Hypotension -usually transient
- Have referring hospital start. At times there may
be resistance secondary to unfamiliarity.
Reassure, educate but get the drip started rather
than wait until the team arrives.
16
Interventions
- Patients saturations remain in the 60s with
bagging. - What are you options?
17
Nitrous Oxide
- Nitrous Oxide. The patient may have a degree of
pulmonary hypertension (or indeed ONLY pulmonary
hypertension). - Adverse effects if patient is co-arctation or
sepsis are low. - Benefits could potentially be high.
18
Maximize Ventilatory Efforts
- Mode of ventilation. This patient may need high
frequency ventilation with Nitrous oxide. - Do NOT get stuck fiddling with the ventilator
with a sick patient. Hand bag and assess
pressure, inspiratory times and compliance. - Switch to ventilator when hand bagging has given
best results and assess. Some patients require
hand bagging for the entire transport. - LISTEN and incorporate the RTs assessment and
recommendations.
19
Interventions
- ABCs
- You assess the tube, suction, breath sounds are
equal with good chest rise. - You are trying Nitrous oxide and hand bagging
with little effect. 02 sats remain in the 60-65
range. End tidal C02 is 30. - Anything more?
20
Moving on.
- You are maximizing your resp. intervention.
- Do not get stuck on one system. Maximize your
interventions and move on. The goal is to
stabilize the patient and commence transport. The
airway is patent you are ventilating well. The
oxygenation may be secondary to a cardiac defect
or pulmonary hypertension that will not be fixed
on transport. - Other interventions may help the resp. status.
- Onto the Circulation.
21
Interventions
- Blood pressure is 50s/30s and stable. Perfusion
is poor and there is a possibility of a
Co-arctation. Of note there are femoral pulses,
the oxygen saturation is matching pre and post
ductal at times. - Ensure access. Place UV line.
- Possible etiologies?
22
Keep Thinking!
- The PDA could be so large that femoral pulses are
palpated even with a coarctation. - OR the diagnosis is incorrect and the poor
perfusion is making the oxygen saturation
unreliable and misleading. - Other possibilities?
23
Differential Diagnosis
- Sepsis- make sure broad spectrum abx are given
- Sepsis with pulmonary hypertension
- Pulmonary Hypertension alone
- Other congenital heart defect
24
Circulation
- Ensure the patient has adequate perfusing volume.
Is the patient third spacing with paralysis? Any
urine output? - Large amounts of fluid are contraindicated in CHF
however if the patient has inadequate perfusing
volume or if sepsis is suspected a fluid bolus
(10-20 cc/kg) may be indicated.
25
Interventions
- Dopamine, Dobutamine, Epinephrine,
Nor-Epinephrine are all options. Which one? When? - Generally if a patient has poor perfusion, is
hypotensive after ensuring there is adequate
perfusing volume pressors are indicated.
26
Pressors
- Effects depend upon the pressor and the receptor.
- Alpha receptors
- Alpha 1 postsynaptic vasoconstriction,
mydriasis, contraction of urethral sphincter - Alpha-2 PRE synaptic. Decrease in noradrenaline
release - Beta-1 (ONE heart). ionotropic effect,
increased rate, increased conduction (esp. at
high doses). - Beta-2 (TWO lungs) vasoDILATION,
bronchodilation, (20 of heart B receptors are
type 2 so cardiac effects less)
27
Dobutamine
- Causes increased contractility (Beta-1 effect)
BUT also can have Beta-2 effects with
vasodilation. - Good for cardiogenic shock but not used as a
first line for septic shock. - Contraindicated in Atrial Fib/Flutter, or
Idiopathic Subaortic Stenosis (increased
contractility causes increased outflow
obstruction)
28
Dopamine
- Variable effects which are dose dependent.
- Recent studies indicating renal dosing may be
well intentioned but without real effect. - Between 5-10 mcg/kg/min beta-1 effects lead to
increased cardiac output. Increased rate cause
some concern for increased oxygen consumption. - Contraindicated in tachyarrythmias, ventricular
fibrillation, pheochromocytoma
29
Milrinone
- Phosphodiesterase inhibitor
- Initial Bolus 50 mcg/kg slowly over 1-2 minutes.
- Maintenance 0.375-0.75 mcg/kg/min
- Ionotrope with little chronotropic activity.
Usually used for cardiac kids. Has pronounced
vasodilatory effect. - Watch potassium especially in patients on
Digitalis. Know the K and correct it BEFORE
starting.
30
Inamrinone (amrinone, Inocor)
- Phosphodiesterase inhibitor. ionotrope but also
chronotrope - Initial Bolus 0.75mg/kg slowly over 1-2 minutes.
- Maintenance 5-10 mcg/kg/min
- Contraindicated any outlet tract obstruction
(worse with increased contractility)
31
Epinephrine/Nor-Epinephrine
- Getting to the kitchen sink.
- Use once adequate perfusing volume is assured and
other methods are not working. - Concern of severe peripheral vasoconstriction,
increased cardiac requirements are usually
overrode by severity of case.
32
Circulation
- Little urine output is noted. One 10cc/kg bolus
given. - If patient paralyzed and third spacing Albumin is
a good choice for volume. - Dopamine is started at 5 mcg/kg/min and patients
blood pressure remains stable, perfusion
improves.
33
Sedation/Paralysis
- Do not rush to sedate and paralyze. Removing
sympathetic tone and potential third spacing can
cause severe blood pressure, cardiac output
issues. - Indications
- Fighting the vent
- All over the bed
- Very touchy with desaturation
- Possible pulmonary hypertension
- Contraindications
- limp patient with hypotension.
- Comfortable patient who may need neurological
assessments.
34
Sedatives/Paralytics
- Versed
- Fentanyl
- Ketamine- yes for asthma, NO for glaucoma, head
trauma or seizure. - Succinylcholine for induction. Not in chronic CP,
burns or crush injuries - Vecuronium for maintenance
- DO NOT forget to re-dose and try to re-dose
before you get back to the ICU so there is not an
awakening on sign over.
35
Re-Assess
- After maximizing oxygenation, ventilation,
circulation step back and reassess. - Think out loud. Go over interventions with the
team elicit suggestions AND implement them. If
you do not think an intervention is warranted
explain why. It makes the plan clear to the team
as a whole.
36
Should I stay or Should I go?
- Case by case but a few general guidelines.
- If there is a clear life saving therapy (surgery,
nitrous oxide) that can be offered by
transporting the patient severely ill patients
can be transported AFTER a clear and informed
consent is signed by the legal guardians. Use
clear language. Do not couch the truth.
37
Stay or go?
- If the patient is actively coding from a etiology
that will not be improved upon by transport
(sepsis, inborn error of metabolism) then the
patient is too ill to transport. - If you believe the patient too unstable call the
ICU attending and discuss the case before
leaving.
38
Transport
- The mother was consented.
- On transport the patients oxygen saturation
improved to 98 both pre and postductal. - Perfusion improved.
- Thoughts?
39
Transport
- The patient may indeed NOT have congenital heart
disease. - Sepsis, Sepsis/Pulmonary hypertension or
Pulmonary Hypertension alone may be at work. - Abx are on board, Nitrous is still on, perfusing
volume is adequate. - Make sure to discuss the evolution of the patient
with the accepting team.