BRINGING YOUR NURSE STAFFING COMMITTEE TO LIFE: Staffing, Scheduling - PowerPoint PPT Presentation
1 / 121
Title:
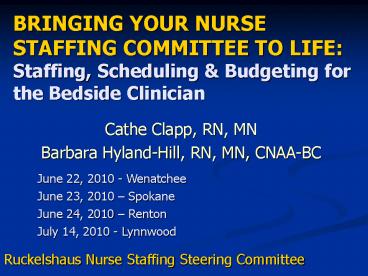
BRINGING YOUR NURSE STAFFING COMMITTEE TO LIFE: Staffing, Scheduling
Description:
BRINGING YOUR NURSE STAFFING COMMITTEE TO LIFE: Staffing, Scheduling & Budgeting for the Bedside Clinician Cathe Clapp, RN, MN Barbara Hyland-Hill, RN, MN, CNAA-BC – PowerPoint PPT presentation
Number of Views:1184
Avg rating:3.0/5.0
Title: BRINGING YOUR NURSE STAFFING COMMITTEE TO LIFE: Staffing, Scheduling
1
BRINGING YOUR NURSE STAFFING COMMITTEE TO
LIFEStaffing, Scheduling Budgeting for the
Bedside Clinician
- Cathe Clapp, RN, MN
- Barbara Hyland-Hill, RN, MN, CNAA-BC
June 22, 2010 - Wenatchee June 23, 2010
Spokane June 24, 2010 Renton July 14, 2010 -
Lynnwood
Ruckelshaus Nurse Staffing Steering Committee
2
WA State Staffing Legislation House Bill 3123
(2008)
- All hospitals must establish a Nurse Staffing
Committee - Composition at least 50 direct care nurses
- Create staffing plans
- If the CEO does not adopt staffing plans, must
provide written explanation - Staffing plans must be posted in public area
- Collect data on 5 NSQI and submit to WSHA
- Report nurse staffing with adverse events
reporting
3
Our Objectives
- Provide you with basic concepts about
- Budgeting (Staffing/Labor Budget)
- Staffing and Scheduling
- Nurse Sensitive Indicators
- Staffing Committee Effectiveness
- Have you apply the concepts
- You leave with a toolkit (tools and resources)
- You will be able to share your learnings with
your committee members (Train the Trainer)
4
Agenda
- Budgeting 101
- Staffing and Scheduling Made Simple
- Nurse Sensitive Indicators for Dummies
- Making the Staffing Committee Work
- Putting It All Together Case Application
5
Budgeting 101
6
Personal Budget
- Income
- Salary Pay check
- Interest/investment earnings
- Expenses
- House payment or rent
- Utilities
- Food
- Insurance
- Car payment
- Gas
- Etc
7
What is a budget?
- A Plan
- Coordination of revenue and expenses
- Specific period of time usually 1 year
- Formalized ? written down
- Forecast the future
An Educated Guess
8
Functions of the Budget
- Financially operationalize an organizations
goals and objectives - Keep management informed
- Evaluate performance
- Refine program development and plan
- Educate
- Increase cost awareness
9
Budgeting Process
- Understand your organizations process, forms,
timeline, terminology, fiscal year - Planning
- Department Goals Objectives
- Projected Units of Service (Volume and Acuity)
- Preparing
- Monitoring and Controlling
- Reporting
10
Staffing Budget(Labor, Personnel, Manpower)
11
Basic Concepts Units of Service
- Unit of Service (UOS) measure of product or
service produced by the department - For Nursing Departments
- Inpatient Units Patient Days
- Outpatient Units Visits
- Emergency Department Visits
- Surgical Units Procedures (Major Minor)
- Minutes
- Labor Delivery Deliveries
- Procedures (Ante partum)
- OP Oncology Treatments
12
The Story of Your Unit
- Who are your patients?
- DRG, age, drugs/therapies/treatments used
- What are their needs?
- Acuity, severity of illness
- What are your hours of operation?
- 24/7
- Other Mon-Fri, 8 am 5 pm
- Collect information on
- Volumes
- Length of stay
- ADT ratio/churn factor
- Number of procedures
- Do you have outpatients or 23-hour stay patients?
- Is the census done at midnight?
13
Basic Concepts Nursing Hours
14
Required Care Hours
- Projected UOS volume
- Determination of workload hours
- Direct nursing care hours per pt day (or UOS)
standard - Patient Classification System Case Mix
- Desired Fixed Staffing Coverage
15
Basic Concepts - FTEs
- FTE Full Time Equivalent
- Equivalent of 1 full-time employee working for 1
year - 1.0 FTE 2080 hrs/yr (8 hrs X 5 days X 52 wks)
- 40 hrs/wk (8 hrs X 5 days)
- 80 hrs/2 wks (8 hrs X 10 days)
- FTEs are converted to positions which are filled
by employees
16
Workload Hours - DNCH
General Medical Unit General Medical Unit General Medical Unit
Bed Capacity 36
Pt Days (UOS) 11,790
ADC occupancy 32.3 89.7 11,790 pt days/365 days 32.3 ADC/36 beds X 100
DNCH/UOS 8.14 Standard
DNCH Required/Yr FTES 95,971 46.1 11,790 pt days X 8.14 DNCH 95,971 hrs/2080
DNCH Required/Day Staff 262.93 32.9 32.3 ADC X 8.14 DNCH 262.93/8 hr shifts
17
Workload Hours - Acuity
Pt Acuity Level DNCHPPD Pt Days Workload Hours
1 3.0 1,061 3,183
2 5.2 3,675 19,110
3 8.8 4,876 42,909
4 13.0 1,704 22,152
5 18.2 474 8,627
Total 11,790 95,981 DNCH 46.1 FTEs
X
18
Workload Hours - Fixed
19
Workload Hours - DNCH
General Surgical Unit General Surgical Unit General Surgical Unit
Bed Capacity 32
Pt Days (UOS) 10,760
ADC occupancy pt days/365 days ADC/36 beds X 100
DNCH/UOS 7.82 Standard
DNCH Required/Yr FTES pt days X DNCH DNC hrs/2080
DNCH Required/Day Staff ADC X DNCH DNC hrs/8 hr shifts
20
Workload Hours - DNCH
General Surgical Unit General Surgical Unit General Surgical Unit
Bed Capacity 32
Pt Days (UOS) 10,760
ADC occupancy 29.5 92 pt days/365 days ADC/36 beds X 100
DNCH/UOS 7.82 Standard
DNCH Required/Yr FTES 84,143 40.5 pt days X DNCH Yearly DNC hrs/2080
DNCH Required/Day Staff 230.69 28.8 ADC X DNCH Daily DNC hrs/8 hr shifts
21
Workload Hours - Allocation
- Staffing Model
- Total pt care, Team, Modular, Primary Care,
Partnership (Dyad) - RN, LPN, NA-C
- Length of shifts 8, 10, 12 hr
- care allocated per shift
22
Required DNC Staff Per Day
General Medical Unit ADC 32.3 DNCH 8.14 Required Hrs 262.93 Required staff 32.9 General Medical Unit ADC 32.3 DNCH 8.14 Required Hrs 262.93 Required staff 32.9 General Medical Unit ADC 32.3 DNCH 8.14 Required Hrs 262.93 Required staff 32.9 General Medical Unit ADC 32.3 DNCH 8.14 Required Hrs 262.93 Required staff 32.9 General Medical Unit ADC 32.3 DNCH 8.14 Required Hrs 262.93 Required staff 32.9
(Hrs by shift) Days 40 (105.17) Eve 30 (78.88) Nights 30 (78.88) Total (by skill mix)
RN (71) 9.3 (105.17 X .71/8) 7.0 (78.88 X .71/8) 7.0 (78.88 X .71/8) 23.3
LPN
NA-C (29) 3.8 (105.17 X .29/8) 2.9 (78.88 X .29/8) 2.9 (78.88 X .29/8) 9.6
Total (by shift mix) 13.1 9.9 9.9 32.9
23
Required DNC Staff Per Day
General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs Required staff General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs Required staff General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs Required staff General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs Required staff General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs Required staff
(Hrs by shift) Days 40 Eve 35 Nights 25 Total (by skill mix)
RN (71)
LPN
NA-C (29)
Total (by shift mix)
24
Required DNC Staff Per Day
General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs 230.69 Required staff 28.8 General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs 230.69 Required staff 28.8 General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs 230.69 Required staff 28.8 General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs 230.69 Required staff 28.8 General Surgical Unit ADC 29.5 DNCH 7.82 Required Hrs 230.69 Required staff 28.8
(Hrs by shift) Days 40 (92.28) Eve 35 (80.74) Nights 25 (40.95) Total (by skill mix)
RN (71) 8.2 (92.28 X .71/8) 7.2 (80.74 X .71/8) 5.1 (40.95 X .71/8) 20.5
LPN
NA-C (29) 3.3 (92.28 X .29/8) 2.9 (80.74 X .29/8) 2.1 (40.95 X .29/8) 8.3
Total (by shift mix) 11.5 10.1 7.2 28.8
25
Required DNC FTEs Per Year
General Medical Unit UOS 11,790 DNCH 8.14 Required Hrs 95,971 Required FTEs 46.1 General Medical Unit UOS 11,790 DNCH 8.14 Required Hrs 95,971 Required FTEs 46.1 General Medical Unit UOS 11,790 DNCH 8.14 Required Hrs 95,971 Required FTEs 46.1 General Medical Unit UOS 11,790 DNCH 8.14 Required Hrs 95,971 Required FTEs 46.1 General Medical Unit UOS 11,790 DNCH 8.14 Required Hrs 95,971 Required FTEs 46.1
Days 40 Eve 30 Nights 30 Total (by skill mix)
RN (71) 13.1 9.8 9.8 32.7
LPN
NA-C (29) 5.4 4.0 4.0 13.4
Total 18.5 13.8 13.8 46.1
26
Required DNC FTEs Per Year
General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs Required FTEs General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs Required FTEs General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs Required FTEs General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs Required FTEs General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs Required FTEs
Days 40 Eve 35 Nights 25 Total (by skill mix)
RN (71)
LPN
NA-C (29)
Total
27
Required DNC FTEs Per Year
General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs 84,143 Required FTEs 40.5 General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs 84,143 Required FTEs 40.5 General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs 84,143 Required FTEs 40.5 General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs 84,143 Required FTEs 40.5 General Surgical Unit UOS 10,760 DNCH 7.82 Required Hrs 84,143 Required FTEs 40.5
Days 40 (33,658) Eve 35 (29,450) Nights 25 (21,035) Total (by skill mix)
RN (71) 11.5 (33,658 X .71/2080) 10.1 (29,450 X .71/2080) 7.2 (21,035 X .71/2080) 28.8
LPN
NA-C (29) 4.7 (33,658 X .29/2080) 4.1 (29,450 X .29/2080) 2.9 (21,035 X .29/2080) 11.7
Total 16.2 14.2 10.1 40.5
28
Non-Productive Hours
- Coverage for anticipated time off (backfill or
replacement) - How does your organization define Non-Productive
Hours? - PTO, Vacation, Sick Leave, Holiday, Bereavement,
FMLA, Education/Professional - What categories of staff must be replaced
- RN, LPN, NA-C, HUC, Monitor Tech, Surgical Tech,
etc
29
Non-Productive Hours
- How does your organization budget for
Non-Productive coverage? - Ave of non-productive time
- Vacation 15 days
- Holiday 9 days
- Average sick 6 days
- Education 2 days
- 32 days 256 hrs (8 hr shift)
- 2080 - 256 1824 prod DNCH
- 256/1825 14
- 46.1 DNC FTEs X 1.14 52.6 46.1 6.5 NP FTEs
30
Non-Productive Hours
- How does your organization budget for
Non-Productive coverage? - Calculate by category of staff replaced and type
of NP time - Vacation
- Sick leave
- Holiday
- Education/Professional leave
- days by staff category X 8 hours X DNC FTE
- 2080
31
Productive Fixed Staff
- Positions whose hours are set and do not adjust
with pt census, volume or acuity - Manager, CNS, Unit-based educator
- Health Unit Coordinator, Monitor Tech
- Need to know
- of days/week and shift coverage
- Are they replaced when off?
32
Non-Productive Impact
FTE NP NP FTE Total FTE
Manager 1.0 - - 1.0
RN 32.7 14 4.6 37.3
NA-C 13.4 14 1.9 15.3
HUC 2.8 14 .4 3.2
Total 49.9 6.9 56.8
33
Indirect Care Hours
- Paid, worked hours related to unit/dept function
- Orientation
- Inservice education CPR, mandatory education
- Staff meeting time
- Shared governance meetings
- Committee time/work
- QA, Clinical Pathways, Standards, etc
34
Indirect Care Hours
- Calculated by type of activity by skill mix
- staff X hrs X times hrs
- Orientation
- Turnover by category
- Anticipated Retirements
- Ave days oriented
- New graduates
- Do you take?
- Do you have a Residency Program? How long is it?
- Are the new graduates hours expensed centrally or
to unit?
35
Indirect Care Hours
Indirect Productive Hours Indirect Productive Hours Indirect Productive Hours Indirect Productive Hours Indirect Productive Hours
Annual Hrs Staff Total Hours FTE
Education and Meetings
RN Education Meetings 40 64 2,560 1.2
NA-C Education Meetings 20 32 640 .3
HUC/MT Education Meetings 20 7 140 .1
Subtotal 1.6
Orientation
RN (average days 15) 120 5 600 .3
NA-C (average days 10) 80 4 320 .2
HUC (average days 15) 120 1 120 .1
Subtotal .6
Total 2.2
36
Staff Per Day FTE Budget
Direct Care Staff/Day 32.9
FTEs
Direct Nursing Care 46.1
Fixed Staff 3.8
14 Non-Productive 6.9
Indirect Time 2.2
Total Paid FTEs 59.0
37
Premium Pay
- Shift differential
- Weekend differential
- Charge nurse, certification, preceptor
differential - Overtime
- Standby and call back pay
38
Basic Concepts Hours Per UOS
- UOS are compared in a ratio to paid or direct
hours required to deliver the service or product - Common Productivity Standard in Nursing
- Nursing Hours Per Pt Day (HPPD)
- Direct Care Hours
- Productive Hours Paid/UOS
- Total Hours Paid/UOS
39
Basic Concepts Formulas
- Average Daily Census (ADC)
- Total pt days
- of days (week, month, year)
- Average Length of Stay (ALOS)
- Total pt days
- of discharges
- Percent Occupancy
- Total pt days Census or ADC
- Total bed days available Beds available
or
40
Basic Concepts Formulas
- Total Direct or Total Productive Hrs/UOS
- Total direct or productive hrs
- Patient days or UOS
- Total Paid Hours/UOS
- Total paid hrs
- Patient days or UOS
41
Basic Concepts Formulas
- Average Hourly Rate
- Total salary
- Total hours paid
- Total Productive Salary Expense/UOS
- Total productive salary
- Patient Days or UOS
- Total Salary Expense/UOS
- Total productive salary
- Patient Days or UOS
42
Sample Cost Center Report
43
Basic Concepts Variance Analysis
- A variance is the difference between the Budgeted
amount and the Actual results - Favorable versus Unfavorable variance
- Variance analysis is a component of budget
monitoring to investigate and explain why
differences occurred - Individual manager accountability for budget
variances
44
Basic Concepts Variance Analysis
- Flexible Budget Variance Analysis
- Variance is a function of
- Volume (output) (Patient Days or UOS)
- Price or Rate (Ave Hourly Rate)
- Quantity or Use (Nursing Hours Used)
- f (Volume Quantity Price)
45
Basic Concepts Staffing Costs
- What affects Staffing Costs?
- Volume (UOS)
- Total Hours Paid
- Direct Care Hrs Pt Acuity, ADT ratio, staffing
to matrix - Indirect Care Hrs Orientation of new staff,
mandatory inservices or meetings - Non-Productive Hrs Sick leave, vacation, FMLA,
holiday - Average Hourly Rate Paid
- Overtime or premium pay situations
- Registry or Traveler use
- Skill mix used
46
Staffing and Scheduling Made Simple
47
Creating Position Control and Schedules
- DEMAND
- Patient Type
- Patient Volume and Acuity
- Demand Variations (churn, time of day, days of
week, months, seasons) - RESOURCES
- Roles (Fixed and Variable)
- FTE Mix
- Days of the week
- Shifts
48
Staffing Model
- Revisit, or build from the ground up, so allows
manager and staff to understand all of the
elements of staffing and resource use - Start with budgeted average daily census
(DEMAND) and the direct care staff FTE budget
(RESOURCES)
48
49
From Budget to a Balanced Schedule you need
- Unit Census and FTE Budget
- Staffing to Census (and Acuity) Matrix
- Core Daily Staffing Model (at census or occupancy
target) - Add in Non Productive FTEs
- Position Control (Personnel Budget)
50
Indirect Care Hours
- Paid hours related to unit/dept function not in
DNCHs - Orientation
- Inservice education CPR, mandatory education
- Staff meeting time
- Shared governance meetings
- Committee time/work
- QA, Clinical Pathways, Standards, etc
51
Staffing Model
Indirect Productive Hours Indirect Productive Hours Indirect Productive Hours Indirect Productive Hours Indirect Productive Hours
Annual Hrs Staff Total Hours FTE
Education and Meetings
RN Education Meetings 40
CNA Education Meetings 20
USMT Education Meetings 20
Total Education and Meetings
EXAMPLE
RN Education 40 73 2920 1.4
Do same for any other identifiable indirect
and/or non-productive hours i.e. vacation
52
Non-Productive Impact
FTE NP NP FTE Total FTE
Manager 1.0 - - 1.0
RN 32.7 14 4.6 37.3
NA-C 13.4 14 1.9 15.3
HUC 2.8 14 .4 3.2
Total 49.9 6.9 56.8
53
Unit Budget Overview
General Medical Unit General Medical Unit General Medical Unit General Medical Unit
Bed Capacity 36 Pt Days (UOS) 11,790
ADC occupancy 32.3 89.7 DNCH/UOS 8.14
DNCH Req/Yr FTES 46.1 DNCH Req/Day Staff/ 8 hours 32.9
Non-Productive FTEs (14) 6.9 Total Unit FTEs 56.8
54
Consider of Days per week to Staff
- 1 FTE needed x days to staff
- of days per week per FTE
- 12 hour shifts .9 FTE x 7 days of staff 2.1
FTE - 3 days per week
- 8 hour shifts 1.0 FTE x 7 days of staff 1.4
FTE - 5 days per week
55
Aim of Improving Staffing and Scheduling Systems
and Processes
- The Right Staff
- In the Right Place
- At the Right Time
- At the Right Cost
- Doing the Right Thing
56
Why is it worth it?
- High quality care
- Eliminating a last minute crisis mode
- Decreases labor intensive re-work
- Agreements between key players
- Reduce use of temporary agency and premium pay
- Support staff satisfaction
57
Why is it worth it?
- To provide high quality care to our patients by
effectively managing our scheduling and staffing
practices. - Move us to more proactive planning and problem
solving with the goal of eliminating a last
minute crisis mode of operation. - Standardize and streamline processes and increase
accuracy which in turn decreases labor intensive
re-work. - Create role agreements between key players that
help make working together more pleasant and
effective. - Reduce use of temporary agency and premium pay in
a sustainable fashion. - Support staff satisfaction with equitable
treatment as well as reasonable and transparent
accommodations when appropriate.
58
Monthly schedules including vacations etc
59
High Level Staffing and Scheduling Overview
60
Overuse of the Word STAFFING
- We are having a 2 hour surge in census every
afternoon from 3 to 5 pm - Our position control is unbalanced. The mix of 8
and 12 hour shifts has weekly gaps in scheduled
coverage from 3 to 7pm - We are scheduling to our average census and are
unable to meet peak patient census days which
have been occurring 17 days per month in the last
6 months.
61
Overview of Three Distinct Staffing and
Scheduling Phases
Scheduling
The Middle
Staffing
Before the schedule is posted
Mid Process Posted to 24-72 Hrs before
24 Hrs before to day of staffing
- Outcome
- Final staffing adjustments
- Float pool assignment
- Outcome
- Re-balancing of
- schedule prn
- Outcome
- -Balanced schedule
- Cost effective plan for
- filling vacancies
- Scheduling Process - from when requests are due
until final schedule posted - Middle Flow - activity after the schedule is
posted -up to 24 hrs before (72 hrs on weekends) - Staffing Process -from 24 hrs before (72 hrs on
weekends) to day of staffing
62
Scheduling Philosophy
- Schedules ensure enough staff with the right
skills to provide safe, quality patient care 24/7
- Schedules are proactive and account for all
direct and non-productive staffing needs
- Effective scheduling models minimize the ultimate
last-minute staffing needs for a shift - Schedules are dynamic and flexible but changes
are minimized
Patient
Scheduler
Manager
Staff
63
What are the characteristics of an effective unit
scheduling process?
- Capable of creating schedules that meet unit
needs - Recognizes importance of stakeholder
relationship and role agreements in scheduling
and staffing processes - Ability to flex schedules (up and down) based on
patient and unit needs - Recognizes unit volumes and workload patterns
- Recognizes special circumstances
- Takes technology into consideration
- Defines options for filling vacancies
64
Scheduling Process Steps
Scheduler Manager Staff
Core and patterns are established Staff submit requests Anticipated monthly variations Schedule adjustment are identified Temporary schedule reviewed Temporary schedule posted Gaps (to core) are filled Final schedule posted Core and patterns are established Staff submit requests Anticipated monthly variations Schedule adjustment are identified Temporary schedule reviewed Temporary schedule posted Gaps (to core) are filled Final schedule posted Core and patterns are established Staff submit requests Anticipated monthly variations Schedule adjustment are identified Temporary schedule reviewed Temporary schedule posted Gaps (to core) are filled Final schedule posted
Important to clarify the roles and
responsibilities of key players in the Scheduling
process
65
Staffing and Scheduling Definitions
Balanced Schedule Nursing units have a pre-defined core number of staff for each day of the week and each shift. This core is based on budgeted HPPD/HPUOS along with expected patient volumes and acuity by day of the week and shift. A balanced schedule meets core staffing levels in the most consistent manner possible i.e. a surgical unit that schedules seven nurses early in the week and two less on weekends because of surgeries occurring early in the week.
Rebalancing The process of exploring and scheduling additional hours to compensate for unplanned uncontrollable changes in scheduled hours and/or volume after the schedule is posted or any time up until the staffing process map begins at 24 hrs (72 hrs on weekends)
Unbalanced Schedule Okay Multiple open positions Not-Okay Granting more than established caps People not working to FTE status Guaranteed patterns that create imbalance Per Diems not working required shifts
Non Productive (NP) Caps Specified amount of NP shifts allowed per schedule. Non-productive hours include vacation and educational meetings.
66
Handy and Very Helpful Definitions
- Scheduling Changes / Trades
- Floating guidelines
- Contracted Agency (local and travelers) and
Extension Contracted - Agency (local and travelers)
- Premium Pay Approval including use of
prescheduled OT / On Call - Posting and offering vacant shifts at straight
time on the unit, division, - system-wide (monthly, weekly and daily)
- Approving vacation requests
- Trades
- Holiday schedules
- Personal Leave
- Expectations for hours worked by per diem staff
- Approving and scheduling non-productive time at
the time of schedule - creation
- Scheduling all FT and PT staff to assigned FTE
- Soliciting voluntary increased hours by PT
staff at FSLA rates of pay
67
ADT Factor AKA Workload Intensity Demand
- The decrease in patient length of stay and the
drive to enhance unit throughput has increased
work activity - The number of admissions, discharges, and
transfers are usually not reflected in patient
classification systems and never in midnight
census - This activity consumes nursing care hours and
must be considered when looking at daily
staffing, particularly in nursing units where
there is high patient turnover
The Hidden Patient Demand
Source Perspective on Staffing Scheduling,
September 2000
68
Calculation of the ADT Factor
- Divide the total number of Admissions,
Discharges, Transfers In Out, and Deaths in a
designated 24-hour period - by the Midnight Census
- to determine the ADT Factor
Source Perspective on Staffing Scheduling,
September 2000
69
ADT Factor - Example
Nursing Unit Number of ADT Midnight Census Unit Specific Score
Unit A 15 12 125 turnover
Unit B 5 25 20 turnover
Source Perspective on Staffing Scheduling,
September 2000
70
ADT Factor - Impact
- Has significant impact on budgeting and staffing
effectiveness - Works out to one hour of care required per
patient turnover (Admission, Discharge, Transfer
In, Transfer Out)
71
ADT Factor - Example
- 2000 patient turnovers per year X 1 hour of care
2,000 additional hours of care needed - 2000/2080 .96 additional FTEs needed to manage
patient turnover requirements
72
ADT Factor Typical Unit Percents
- Medical/Surgical 50 - 55
- Telemetry 70 - 75
- Critical Care 85 - 90
- Post Partum 85 - 90
- Mental Health 40
- Rehab 25 - 30
- Source Perspective on Staffing Scheduling,
September 2000
73
Unscheduled Absences
- Most common staffing problem
- Utilization of unscheduled time is increasing
- Very costly Every year, unscheduled absences
costs 2,650 per salaried worker and 3,600 per
hourly worker - Essential to monitor each pay period
Shiftwork Practices 2005, Circadian
Technologies, as cited in Bureau of National
Affairs, Inc., Absence Management Making the
Critical Shift from Transactional to Strategic,
2006.
74
Unscheduled Absence Monitoring
- What staffing response does each unit have
available to respond effectively to unscheduled
absences? - Overtime most commonly used as a response to
deficit demands - Evidence growing that overtime adversely impacts
patient safety and quality of care
75
Overtime Monitoring
- Guideline for overtime use is to keep it less
than 5 of worked hours - Overtime between 5 8 is symptomatic of
financial distress - Overtime greater than 8 is symptomatic of
serious distress
76
Overtime Monitoring
- IOM report recommended limiting work hours to not
more than 12 hours per day and not more than 60
hours per week as a safety measure - In the U.S., many states have legislated No
Mandatory Overtime as a result of patient safety
issues
77
Staffing Plan - Example
Winchester Hospital, MA Medical Unit
Patient Care Link - http//www.patientsfirstma.org
78
Staffing Plan - Example
Winchester Hospital, MA Medical Unit
Patient Care Link - http//www.patientsfirstma.org
79
Nurse Sensitive IndicatorsFor Dummies
80
What we know
- Preventable medical errors cost US healthcare
system 17 billion/year (IOM) - Medication errors cost nearly 3.5 billion/year
(IOM) - Medical errors cause 195,000 deaths/ year in
the US (Health Grades)
81
Nursing Impact on Pt Outcomes
- There is a clear link between nurse staffing
(ARNPs and RNs) and patient outcomes - RNs are the surveillance system for early
detection and intervention for adverse outcomes - Institutional advocate for patient centeredness
- The environment of practice is critical to safety
82
Nursing Impact on Pt Outcomes
- A study of medication errors in 2 hospitals over
6 months showed nurses were responsible for
intercepting 86 of all medication errors before
error reached the patient (Leape et al., 1995) - Leaner RN staffing/less RN hrs of care are
associated with - ? LOS (AHRQ, 2001 Needleman et al., 2002, 2006)
- Nosocomial infections (UTI, post-op infection,
pneumonia) (AHRQ, 2001 Needleman et al., 2002,
2006 Aiken et al., 2002) - Pressure ulcers (AHRQ, 2001)
- GI bleeding (Needleman et al., 2002, 2006)
- Cardiac arrests (Needleman et al., 2002, 2006)
- Patient deaths (Needleman et al., 2002, 2006
Aiken et al., 2002)
83
Thus, what we know.
- Nurses Patient Safety
- Nurses Quality Outcomes
- Quality Cost Effective Care
- Outcomes
84
Staffing Indicators
- NHPPD
- On call/per diem use
- Overtime
- Sick time
- Skill mix
- Agency hours
- Sitter hours
- Meal breaks
- Staff injuries
- Staff satisfaction
- Staff turnover rate
- Staff vacancy rate
- Understaffing compared to staffing plan
- Practice environment scale
National Quality Forum endorsed Nursing
Sensitive Indicators
85
Clinical Indicators
- Patient falls
- Patient falls with injury
- Pressure ulcer
- Infection rates
- Urinary tract
- Postoperative
- Central line
- Ventilator related
- Pneumonia
- Adverse drug events
- Injuries to pts
- Upper GI bleeding
- Shock/cardiac arrest
- Length of stay
- Failure to rescue
- Restraint prevalence
- Smoking cessation
- AMI, CHF, Pneumonia
National Quality Forum endorsed Nursing
Sensitive Indicators
86
Service Outcomes
- Patient satisfaction score
- Patient complaints
- Family complaints
- Patient satisfaction with pain management
- Patient satisfaction with ability to manage care
at home (patient teaching/education) - Patient satisfaction with nursing and overall care
87
Core Measures (JCAHO)
- Surgical Care Improvement Project (SCIP)
- Heart Failure
- AMI
- Pneumonia
- Pregnancy
- Childrens Asthma Care
- Hospital Inpatient Psychiatric Services
88
CMS Non-Reimbursed Conditions
- Preventable Hospital-Acquired Conditions
- Object left in pt during surgery
- Air embolism
- Blood incompatibility
- Catheter-associated urinary tract infection
- Pressure ulcer
- Vascular catheter-associated infection
- All surgical site infections
89
CMS Non-Reimbursed Conditions
- Preventable Hospital-Acquired Conditions
- Falls with injuries
- Ventilator associated pneumonia
- Staphyloccus aureus septicemia
- Deep vein thrombosis and pulmonary embolism
- MRSA
- Clostridium difficile-associated disease
- Wrong surgery
90
Benchmarking and Reporting
- National Database of Nursing Quality Indicators
(NDNQI) - Collaborative Alliance of Nursing Outcomes
(CALNOC) - Washington State Hospital Association
91
WA State - NSQI
- Falls
- Falls with injury
- Pressure ulcers
- Nursing hours per patient day
- Skill mix
92
Cost Factors Related to Pt Safety
- Occurrence of the medical error
- Prevention of the medical error
- Treatment of the medical error
Pay Now or Pay Later
93
Where to start.
- Collect the data
- What data are being tracked now?
- Unit/department level
- Organization wide
- Frequency of data collection
- Reports available
- Analyze the data
- Trends
- Comparison to benchmark data
- Questions to ask
- Make the data visual and available
- Identify patterns or improvement opportunities
94
Sample Nursing Scorecard
95
Performance Measure Example
Patient Care Link - http//www.patientsfirstma.org
96
Performance Measure Example
Patient Care Link - http//www.patientsfirstma.org
97
Performance Measure Example
Patient Care Link - http//www.patientsfirstma.org
98
Professional Nursing Organizations - Recommended
Staffing Standards
WSNA, 2010 - www.wsna.org/Topics/Safe-Nurse-Staffi
ng/Toolkit/Documents/Staffing-Ratio-Grid.pdf
99
Professional Nursing Organizations - Recommended
Staffing Standards
WSNA, 2010 - www.wsna.org/Topics/Safe-Nurse-Staffi
ng/Toolkit/Documents/Staffing-Ratio-Grid.pdf
100
Making the Staffing Committee Work
101
Too many meetings?
Team building and conflict resolution Problem solve
Set goals and make plans Accountability and tracking progress
Share content Share content
102
Meeting Tools
- Team Charter
- Ground Rules for Teams
- Meeting Roles
- Agenda
- Minutes
- Evaluations
103
Type of Meetings
- Hospital-wide
- Unit based
- Multidisciplinary
- that can be.
- Short term projects
- Ongoing standing committees
- Focused sub-committees
Tools work for all types of meetings
104
Committee Charter Elements
- Purpose and Goals
- Membership and Sponsorship
- Boundaries
- Decision Making and Levels of Authority
- Roles and Responsibilities
- Ground Rules / Team Agreements
- Meetings and Communications
- Measures of Success
Go Slow to Go Fast
105
Levels of Involvement
Communication Participate in developing
solutions, changes and proposals. Opportunity to
influence through giving feedback on what is
already designed. Opportunity to influence final
decision participate in monitoring and taking
corrective action. Full partners in reaching
final decisions, formulation plans, monitoring
and taking corrective action.
Informed
1 2 3 4 5
Consulted
Developers
Input on Decision Making
Full Decision Making Authority
106
Other Supporting Stakeholders
- Medicine
- Ancillary and Support Departments
- HR
- Finance
- Quality
- Staffing Office
- Medical Records
- Communication and Marketing
107
Agendas
- Published prior to meeting to each member
- Established at previous meeting
- Includes members names next to assigned agenda
item - Includes time allotment for each topic
108
Effective Agendas
- Review objectives
- Review agenda items
- Work through agenda items
- Review assignments
- Plan for next meeting
- Rate effectiveness of meeting
109
Minutes Official Record
- List who was present (and who was absent if group
membership is defined) - Summary of decisions made for each agenda item
- List assignments
- Next meeting time and location
- Published within a week
Tailor to Your Needs Legal? Functional?
Communication Tool?
110
Team Ground Rules
- - Key -
- Established by Committee!
111
Ground Rules for Good Teams
- Assumption that each person wants to be here
- Team members speak freely and in turn
- All team members and opinions are equal
- If you have something to say, say it in the room
No Meetings After the Meeting - No sidebar communications
- Each one must be heard - others listen
attentively - No one may dominate - no whining
- Problems are discussed, analyzed or critiqued,
not people - Honesty before cohesiveness
- Consensus is the goal--finding solutions
acceptable to everyone I can support this even
if it isnt the ideal solution - Silence is not understood to equal agreement.
Making a request for someones point of view is
acceptable. - All agreements are kept unless renegotiated
- Once agreement occurs, speak with ONE VOICE
112
Ground Rules for Good Meetings
- Meeting frequency and length defined
- Start and end on time
- Come prepared do homework
- Members must attend regularly
- Stay on target
- Leave rank at the door
- At least one bright idea per session
- Identify problems and focus on solutions input,
discussion, decision - Review the objectives before we leave realistic
in scope - Leave with a sense of accomplishment a purpose,
making a difference - Expect work outside of the meeting subgroups
and task forces
113
Important Meeting Roles
- - Co-Chairs-
- Opens the meeting
- Reviews the agenda
- Makes sure someone is taking notes keeping
track of time - Moves through the agenda one item at a time
- Keeps the team focused
- Establishes an appropriate pace
- Facilitates discussion and manages participation
- Helps the team use appropriate decision-making
methods - Helps the team evaluate the meeting
- Gathers ideas for the next meetings agenda
- Closes the meeting
(from The Team Handbook)
114
Important Meeting Roles
- Notetaker
- Records minutes which include key topics, points
made during discussion, decisions made, actions
items (who will do what, and by when) - Rotate turns taking minutes / seek secretarial
support - Send minutes to Co-Chairs for review then
distribute the minutes within one week of the
meeting
(from The Team Handbook)
115
Important Meeting Roles
- - Timekeeper -
- Keeps track of time to help team move along
- Alerts the team when the allotted time is almost
up so that the team can decide whether to
continue discussion or table it
(from The Team Handbook)
116
Important Meeting Roles
- - Discussion Scribe -
- Posts ideas on a flipchart or whiteboard
- Write legibly and large enough so that all can
see - Captures issues that do not directly relate to
the topic on a parking lot (separate flip chart
page)
(from The Team Handbook)
117
Communications
- Between committees vertical and horizontal
- Between co-chairs and members of committees
- Between stakeholders and committees
- Members at large
- Multiple modalities
- Over communicate You are Educating a parade!
118
Sources of Data and Examples
Your committee is ready for data?
Staffing/Scheduling Core staffing structure Low Census days
Medical Records Documentation compliance Length of stay
Unit/Department ER Left without being seen OR Case start times Patient satisfaction
119
Sources of Data and Examples
Financial / Budget Cost per patient day Volume or Units of service
Payroll Absences Overtime Hours
Human Resources Vacancies and Turnover Full Time/ Part Time Mix
Quality Medication errors Infection rate Patient falls
120
Putting it All TogetherCase Application
121
Putting it All Together Case Applications
- Budgeting Scenario
- Staffing and Scheduling Scenario
- Creating a Council Charter
- Workforce Planning Assessment
- Staffing Committee Survey
- Quality Scenario