I.Introduction - PowerPoint PPT Presentation
Title:
I.Introduction
Description:
H. Conditioned place ... ACC, anterior cingulate cortex; CC, corpus callosum; FC, frontal cortex; HC, hippocampus; HY ... One compartment has a grid floor ... – PowerPoint PPT presentation
Number of Views:143
Avg rating:3.0/5.0
Title: I.Introduction
1
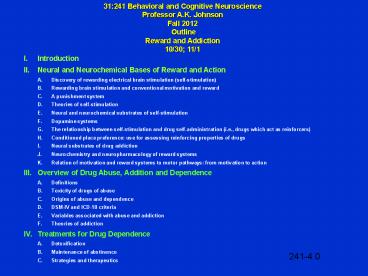
31241 Behavioral and Cognitive
NeuroscienceProfessor A.K. JohnsonFall 2012
OutlineReward and Addiction10/30 11/1
- I. Introduction
- II. Neural and Neurochemical Bases of Reward and
Action - A. Discovery of rewarding electrical brain
stimulation (self-stimulation) - B. Rewarding brain stimulation and conventional
motivation and reward - C. A punishment system
- D. Theories of self-stimulation
- E. Neural and neurochemical substrates of
self-stimulation - F. Dopamine systems
- G. The relationship between self-stimulation and
drug self-administration (i.e., drugs which act
as reinforcers) - H. Conditioned place preference use for
assessing reinforcing properties of drugs - I. Neural substrates of drug addiction
- J. Neurochemistry and neuropharmacology of
reward systems - K. Relation of motivation and reward systems to
motor pathways from motivation to action - III. Overview of Drug Abuse, Addition and
Dependence - A. Definitions
- B. Toxicity of drugs of abuse
- C. Origins of abuse and dependence
- D. DSM-IV and ICD-10 criteria
- E. Variables associated with abuse and addiction
241-4.0
2
Key Terms and Concepts
Abstinence syndrome Dependence Depressant (neural
depressant) Dorsal mesostriatal (nigrostriatal)
Drug abuse Drug sensitization Drug
tolerance Mesocortical
Mesolimbic Naloxone Nigrostriatal Sensitization St
imulants Tolerance Ventral mesostriatal
(mesolimbic) Ventral pallidum
241-4 KTC
3
Operant Chamber (Skinner Box)for Delivery of
Rewarding ElectricalBrain Stimulation
(Self-Stimulation)
241-4.1
4
A Cumulative Bar-Pressing Curve for a
Self-Stimulating Rat With an Electrode in a
Positive Reward Site
241-4.2
5
The Relationship Between Self-Stimulation and
Conventional Motivated Behaviors and Reward
Performance on instrumental tasks - Reward
magnitude - Priming - Rapid extinction -
Schedules of reinforcement - Chaining of
behaviors - Secondary reinforcers
Electrically elicited behaviors (drinking,
eating, chewing, hoarding, aggressive
reproductive responses) Aversion/punishment
systems
241-4.3
6
Some Sites Which Support Intracranial
Self-Stimulation in Various Animal Species
Brain Area Sites Which Support
Self-Stimulation Forebrain Frontal
cortex Entorhinal cortex Olfactory
nucleus Caudate nucleus Nucleus
accumbens Entopeduncular nucleus Septal
area Hippocampus Amygdaloid nucleus Ventral
and medial thalamus Hypothalamus Median
forebrain bundle Dorsal noradrenergic
bundle Midbrain and Ventral tegmental
area Substantia nigrabrain stem Raphe
nuclei Nucleus coeruleus Superior
cerebellar Periaqueductal gray matter
peduncle Mesencephalic nucleus of
trigeminal nerve Cerebellum Deep cerebellar
nuclei Other cerebellar areas Medulla Motor
nucleus of trigeminal nerve Nucleus of
tractus solitarius
241-4.4
7
Neuroanatomy of Brain Rewardand Punishment
Systems
241-4.5
8
Theories of Self-Stimulation
Automatistic behavior Hedonic (Olds)
Dual activation of drive and reward pathways
(Deutsch Gallistel) Consummatory behavior
(Glickman Schiff) Incentive motivation
(Trowill, Panksepp Gandelman)
241-4.6
9
Lines of Evidence Supporting the Idea that
Catecholamines (CAs) Mediate Rewarding Brain
StimulationLarry Stein(Circa 1966)
Drugs that facilitate self-stimulation release
CAs (e.g., amphetamine). Drugs that inhibit
self-stimulation deplete CAs (reserpine,
?-methyl-p- tyrosine). Drugs that block
adrenergic transmission (chlorpromazine) inhibit
self-stimulation. Protection of CAs with
monoamine oxidase inhibitors or block reuptake
(e.g., imipramine) enhances the facilitatory
effect of amphetamine on self-stimulation.
Depletion of brain CAs with reserpine or
?-methyl-p-tyrosine decreases the
facilitatory effects of amphetamine on
self-stimulation. A large component of the
medial forebrain bundle (MFB), a hot-spot for
self-stimulation, is catecholaminergic.
Rewarding stimulation of the MFB causes release
of norepinephrine into the amygdala and
hypothalamus.
241-4.7
10
Horizontal and Lateral Representations of
Ascending Noradrenaline and Dopamine Pathways
241-4.8
11
Dopaminergic Pathways in the Rat Brain
241-4.9
12
The Four Major DA Pathways in the Brain
241-4.10
13
Brain Dopamine Systems
Ultrashort Retina interplexiform
amacrine-like neurons Olfactory bulb
periglomerular dopamine cells Intermediate
Length Tuberohypophyseal
Incertohypothalamus Medullary
periventricular Long Length Nigrostriatal
Mesolimbic Mesocortical
241-4.11
14
The Dopamine Synapse
241-4.12
15
Six Types of Postsynaptic Dopamine Receptors
D1 and D5 D2a D2b
D3 and D4 Molecular structure Seven
membrane- Seven membrane- Seven membrane- Seven
membrane- spanning regions spanning
regions spanning regions spanning
regions Effect on cyclic AMP Increases Decreases
Increases phospho- ?
inositide turnover Agonists Dopamine Full
agonist (weak) Full agonist (potent)
Apomorphine Partial agonist (weak) Full agonist
(potent) Antagonists Phenothiazines Potent Po
tent Thioxanthenes Potent Potent
Butyrophenones Weak Potent Clozapine Inactive
Weak Weak Potent
241-4.13
16
The Rotometer
241-4.14
17
Investigation of the Actions ofDopamine in the
Nigrostriatal SystemDrug-Induced Rotational
Behavior in Rats with Unilateral Nigrostriatal
Lesions
241-4.15
18
Some Prototypic Dopamine Agonists and Antagonists
Presumed Mechanism Most Prominent Drug
of Action Physiological
Effects Antagonists Butyrophenones
Haloperidol Phenothiazines Receptor
blockade Tranquilizer antipsychotic
antinauseant Chlorpromazine Agonists
Apomorphine Receptor stimulation Antiparkinsonian,
emetic Bromocriptine Releasers
Amphetamine Releaser Stimulant, appetite
suppressant Vesicular Storage Inhibitors
Reserpine Depletion Antihypertensive
tranquilizer antipsychotic Pump
Inhibitors Cocaine Reuptake inhibition Stimulan
t euphoriant Synthesis Inhibitors
Carbidopa Dopa decarboxylase inhibition Adjuvant
for central dopa ?-Methyl-p-tyrosine Tyrosine
hydroxylase inhibition Depressant
akinesia Monoamine Oxidase Inhibitors
Iproniazid Broad-spectrum MAO inhibition Antidepr
essant COMT Inhibitors Tropolone,
pyrogallol, COMT inhibition Minimal effects
rutin, quercetin False Transmitters
?-Methyldopamine Antihypertensive Toxin
6-Hydroxydopamine Destruction of
cells Experimental Precursors Dopa Stimulates
transmitter production Antiparkinsonism and mild
stimulant Also has prominent norepinephrine or
epinephrine action, or both
241-4.16
19
The Medial Forebrain Bundle is One of the
"Hottest" Brain Pathways for Self-Stimulation
241-4.17
20
Blockade of Medial Forebrain Bundle
Self-Stimulation by Dopamine Receptor Antagonist
Infused Into the Nucleus Accumbens
241-4.18
21
Effects of Electrical Self-Stimulationof the
Ventral Tegmental Area on Extracellular Dopamine
in the Nucleus Accumbens
241-4.19
22
Apparatus for Producing andMeasuring a
Conditioned Place Preference
241-4.20
23
Place Conditioning With Dopamine AgonistsInfused
Into the Nucleus Accumbens
241-4.21
24
Intravenous Self-Administration of Drugs of Abuse
241-4.22
25
Some Drugs Which Act asReinforcers in Animal
Species
Alcohol Marijuana Amphetamines Methadone Apomorphi
ne Methyl phenidate Barbiturates Morphine Benzodia
zepines Nicotine Chlorphentermine Nitrous
oxide Chloroform Pentazocine Clortermine Phencycli
dine Cocaine Phenmetrazine Codeine Pipradrol Dieth
ylpropion Procaine Ether Propiram Lacquer,
thinners Propoxyphene Animals will voluntarily
self-administer these drugs after suitable
priming, depending on dose, schedule, route of
administration, and species. Routes of
administration include intravenous,
intramuscular, inhalation, intracerebral,
intragastric tube, and oral. Animal species
include rat, monkey, ape, baboon, dog, and
others.
241-4.23
26
Mediation of the Rewarding Effects of Drugs of
Abuse by Dopamine (DA) Action in the Nucleus
Accumbens
241-4.24
27
Hypothesized Sites of Action of Drugson
Brain-Reward Circuitry in the Rat
241-4.25
28
Changes in Dopamine Detected in the Extracellular
Fluid of the Nucleus Accumbens of Rats After
Daily Intraperitoneal Cocaine Injections (10
mg/kg)
241-4.26
29
Tetrahydrocannabinol (THC)-Induced Enhancementof
Dopamine Efflux in the Nucleus Accumbens
241-4.27
30
Two Systems Responsible for theInitiation of
Movements (Actions)One Involves Cognitive
Processes and the Other Involves Those in
Response to Basic Motivations (Drives) and
Emotions
Caudate N. (Neostriatum)
Globus Pallidus
N. Accumbens (Ventral Striatum)
Cerebral Cortex
Limbic Structures
DAA10
VTA
MotorSystem
241-4.28
31
Locomotion Occurs When Inhibitory GABA-Secreting
Synapses on Neuronsin the Globus Pallidus
Decrease Their Activity
241-4.29
32
The Motive Circuit "Translates" thePerception of
a Reward Into Locomotion
241-4.30
33
Simplified Diagram of CentralPathways
Controlling Locomotion
Thalamus
NRP
NRP
Spinal Pattern Generator
Caudate N.(Neostriatum)
Mesencephalic Locomotor Region(Pedunculo Pontine
Nucleus)
Globus Pallidus
Cerebral Cortex
VentromedialMedulla
N. Accumbens (Ventral Striatum)
Limbic Structures
MotorSystem
VTA
VTA, ventral tegmental area NRG, nucleus
reticularis gigantocellularis NRP, nucleus
reticularis pontis oralis
241-4.31
34
Drug Dependence and Abuse
Drug Abuse a maladaptive pattern of substance
use manifested by recurrent and significant
adverse consequences to repeated use of
substances. Dependence Drug dependence is a
state whereby an individual either psychologicall
y or physically requires a drug in order to feel
well in the absence of medical indications.
Discontinuation of the drug will produce a
characteristic group of withdrawal symptoms.
Physiological dependence adverse
physiological reactions (e.g., stomach cramps)
in the absence of drugs. Primary
psychological dependence produces
pleasure and/or reduces "psychic" discomfort
(drug craving). Secondary psychological
dependence fear or anxiety as a result of a
lack of drug.
241-4.32
35
Drug Addiction Substance Dependence
- 1. Compulsion to seek and take a drug.
- 2. Loss of control in limiting intake.
- 3. Emergence of negative emotional state (e.g.,
dysphoria, anxiety, irritability) when access to
drug is prevented. - 4. Chronic relapsing disorder.
241-4.33
36
Categories of Drugs of Abuse
Opiates and Opioids Morphine, codeine, heroin,
meperidine, hydromorphone, and other opioid
agonists Stimulants Cocaine, amphetamines,
methylphenidate, nicotine, caffeine Depressants
Barbiturates, non-barbiturate sedatives,
benzodiazepines, and ethanol Hallucinogens
D-lysergic acid diethylamide (LSD), mescaline,
methylenedioxymethamphetamine (MDMA),
phencyclidine, marijuana Inhalants
241-4.34
37
Classification of Drug Use
- 1. Occasional, controlled, social use
- 2. Abuse or harmful use
- 3. Addiction
241-4.35
38
Drug Use, Abuse and Dependencein U.S. Adults
- At Some Point in Their Lifespan
- 15.6 engage in illicit drug use
- 3.1 engage in abuse
- 2.9 develop dependence
241-4.36
39
DSM-IV and ICS-10 Diagnostic Criteria for Alcohol
and Drug Abuse/Harmful Use
DSM-IV Alcohol and Drug Abuse A. A maladaptive
pattern of substance use leading to clinically
significant impairment or distress, as manifested
by one (or more) of the following, occurring
within a 12 month period 1. Recurrent substance
use resulting in a failure to fulfill major role
obligations at work, school, or
home. 2. Recurrent substance use in situations
in which it is physically hazardous. 3. Recurrent
substance-related legal problems. 4. Continued
substance use despite having persistent or
recurrent social or interpersonal problems
caused or exacerbated by the effects of the
drug. B. The symptoms have never met the criteria
for substance dependence for this class of
substances. ICD-10 Harmful Use of Alcohol and
Drugs A. A pattern of substance use that is
causing damage to health. The damage may be
physical or mental. The diagnosis requires that
actual damage should have been caused to the
mental or physical health of the user. B. No
concurrent diagnosis of the substance dependence
syndrome for same class of substance.
241-4.37
40
DSM-IV and ICD-10 Diagnostic Criteria for Alcohol
and Drug Dependence
241-4.38
41
Stages of Drug Addiction/Dependence
241-4.39
42
Diagnostic Criteria of Addiction
- Shift in emphasis in diagnostic criteria from
focus on tolerance and withdrawal to criteria
related to compulsive use. - Diagnostic and Statistical Manual of Mental
Disorders DSM-IV (American Psychiatric
Association) - International Statistical Classification of
Diseases and Related Health Problems ICD-I0
(World Health Organization)
241-4.40
43
Origins of Abuse and Dependence
Drugs that affect behavior are likely to be
taken in excess when the effects are considered
pleasurable. Legal prescription drugs (e.g.,
barbiturates, morphine, amphetamine), illegal
drugs (e.g., heroin and cocaine) and
non-prescription drugs (e.g., ethanol and
nicotine) are abused and can produce
dependence. Very few individuals begin
addiction problems by misuse of prescription
drugs. However, prescribed medications for
pain, anxiety and even hypertension commonly
produce tolerance and physical dependence. Toler
ance and physical dependence do not imply abuse
or addiction.
241-4.41
44
Vulnerability to Addiction
- Individual Differences
- Temperament--Disinhibition--Negative
affect--Novelty/sensation seeking - Social Development--Early drug/alcohol
exposure - Co-morbidity--Mood disorders--Anxiety
disorders--Antisocial personality
disorder--Conduct disorders - Genetics--Contributes to 40 of total
variability associated with drug dependence - Protective Factors--Also receives
contributions from genetics, personality, and
environment
241-4.42
45
Abstinence Syndrome
Physiological and psychological
dependence-related symptoms and signs that arise
during withdrawal of a drug. - Relationship
with ½ life of drug.
241-4.43
46
Relationship Between the Intensity of a Drug's
Effects and the Intensity of the Abstinence
Syndrome
241-4.44
47
Differences in Responsesto Heroin and Methadone
241-4.45
48
Medical/Psychological Views of Addiction
- 1. Dependence ('40's)
- --Physical dependence the sine qua non of the
abstinence syndrome - --Evolved to include "psychic" (psychological)
dependence - --Drug craving
- 2. Psychiatric
- --Addiction has aspect of impulse control
disorders and compulsive disorders - --Impulsive acts preceded by tension or arousal
followed by pleasure gratification or relief - --Compulsive acts preceded by anxiety and stress
followed by relief from stress - --Addiction considered to shift from an
impulsive disorder to a compulsive disorder - --A circle of addiction with 3 stages
preoccupation/anticipation ? binge/intoxication ?
withdrawal/negative affect - 3. Psychodynamic
- --Focuses on developmental difficulties,
emotional disturbances, structural (ego) factors,
personality organization and building of the self - --Associated with a self-medication hypothesis
where users are considered to take drugs to cope
with painful/threatening emotions - --Opiates for anger and rage
- --Psychostimulants for anhedonia, anergia, and
lack of feelings - --Neurodepressants for those flooded by or cut
off from feelings - --Each drug class serves as an antidote for a
dysphoric condition or state - 4. Social Psychological/Self-Regulation
- --Failure in self-regulation leads to addiction
241-4.46
49
Diagram Representing a Psychiatric View of the
Transition of a Problem of Impulse Control to a
Problem of Compulsion in the Course of Becoming
Addicted and the Nature of Reinforcement
(Positive to Negative)
241-4.47
50
Primary Goal of Neurobiological Addiction
Research
- To Understand the Neuropharmacological and
Neuroadaptive/Neuroplastic Mechanisms Within the
neurocircuitry mediating the transition between
occasional drug use and the loss of control over
drug seeking and taking (i.e., addiction).
241-4.48
51
Major Issues for a ComprehensiveUnderstanding of
Drug Addiction
Reward mechanisms Changes in response to the
drug (sensitization or tolerance) Drug
craving Causes for relapse
241-4.49
52
Neuroadaptation Views of Addiction
- 1. Behavioral Sensitization
- ? Berridge Robinson
- ? Conceptually tied to psychomotor sensitization
- ? Incentive sensitization
- ? Liking and wanting
- ? Incentive-salience
- --Cues associated with drug cues and drug
taking become associated through Pavlovian
stimulus associative conditioning to enhance
motivation - 2. Opponent-Process or Counteradaptation Theory
- Contributors used such theories to account
for tolerance and withdrawal - ? Himmelsbach ('40's)
- ? Martin ('60's)
- ? Solomon Corbit ('70's)
- ? Koob Bloom ('80's)
- --Theorized that the brain uses negative
feedback mechanisms to keep affective responses
in check - --An unconditioned "a" process
(positive/pleasurable) is counteracted by a "b"
process - --The "b" process has a larger latency of onset
and duration of action - --"b" process grows disproportionally compared
to the decreasing "a" process and is associated
with an aversive craving state - --Solomon argues that the 'b" process "grows"
with repeated drug taking - 3. Motivational
241-4.50
53
Robinson and Berridge's Theoryof Incentive
Salience and Drug Addiction
Administration of some classes of abused drugs
(e.g., psychostimulants) produce sensitization
(i.e., reverse tolerance). For example,
psychomotor stimulants increase locomotor
behavior with spaced, repeated administration in
a normal environment. Robinson and Berridge
propose that increased drug craving is the
produce of a similar sensitization process where
"wanting" the drug is enhanced.
241-4.51
54
Berridge and Robinson's Model Focusing on the
Role of Incentive Salience as a Factor Related to
Drug Craving and In Turn Relapse
241-4.52
55
The Opponent-Process Theoryof Motivation and
Emotion
241-4.53
56
Koob and Le Moal's Application ofOpponent-Process
Theory to Phenomenology Associated with Drug
Addiction
241-4.54
57
Koob and Le Moal's Diagram of theHypothetical
Spiraling Distress-AddictionFrom a
Neurobiological Perspective
241-4.55
58
Nestler's Theory of Sensitization as aResult of
Drugs that Release DopamineCausing Increased
Fos-Related Antigens (Fra)
241-4.56
59
Behavioral and Cellular/Molecular Changes
Associated with Drug Use, Addiction, Withdrawal
and Long-Term Abstinence
241-4.57
60
Treatment for Drug Dependence
Will vary with the drug being used and social
and cultural factors determining the use. The
management of withdrawal syndromes can be
achieved with minimal risk and high probability
of success using pharmacological agents.
241-4.58
61
Detoxification Withdrawal of Opioids
Most patients will perceive withdrawal
symptoms. May be possible to reduce the
drug. Methadone is suitable for suppressing
withdrawal symptoms. With methadone
substitution in an in-patient setting, symptoms
usually aren't worse than "flu-like"
syndrome. Under these "drug weaning"
conditions, most patients can be withdrawn in
less than 10 days. Clonidine (?2-adrenergic
receptor agonist) can suppress some components of
opioid withdrawal. Clonidine suppresses
autonomic signs and symptoms (e.g., nausea,
vomiting, diarrhea) then drug craving.
241-4.59
62
Withdrawal of Neurodepressants
Abrupt neurodepressant withdrawal can be
fatal. Pentobarbital can be substituted for
any neurodepressant. Pentobarbital is
administered to induce mild intoxication and
maintained 24 to 36 hrs and stabilized, then
withdrawal can be started.
241-4.60
63
Role of PharmacologicalAgents Following
Withdrawal
Therapeutics may be used to treat underlying
psychological problem (e.g., anxiety or
depression). Therapeutic agents intended to be
a less toxic substitute (e.g., methadone) may be
used. Drugs to interfere with reinforcing
actions of the abused drug (e.g., naltrexone).
241-4.61
64
Pharmacological Approach toCocaine and
Amphetamine Dependence
Most consistent pharmacotherapy has been
obtained with tricyclic antidepressants (e.g.,
desipramine). After 1 to 2 weeks, desipramine
appears to reduce craving for cocaine. It is
postulated that the antidepressants increase
functional activity in reward systems by altering
cocaine-induced supersensitivity at dopamine
autoreceptors.
241-4.62
65
Drugs of Abuse and How Their EffectsMight
Theoretically Be Treated
- Mechanism Main Neurotransmitter Involved
Affected Potential Treatment - Action on endogenous receptors for endogenous
ligandsOpioids Endorphins, enkephalins Partial
agonist (e.g., buprenorphine) Antagonists
(e.g., naltrexone) - Alcohol GABA, endorphins Partial agonists (e.g.,
bretazenil) Opiate antagonists (e.g.,
naltrexone) - Benzodiazepines GABA Partial agonists (e.g.,
bretazenil barbiturates Antagonists (e.g.,
flumazenil) - Nicotine Acetylcholine Antagonists (?
mecamylamine) - Cannabinoids ? Anandamide Antagonists (e.g., SR
141716A) - LSD and related 5-HT 5-HT2 receptor antagonists
hallucinogens (e.g., ritanserin) - Increasing the release of endogenous
neurotransmittersCocaine Dopamine D2 receptor
antagonist Antagonist of the uptake site
(e.g., SSRI) - Solvents ? Noradrenaline ? Receptor antagonists
- Antagonizing the action of natural
transmittersAlcohol Glutamate NMDA antagonists
(e.g., dizocilpine) - Most typical (e.g., haloperidol) and atypical
(e.g., sulpiride, tiapride, risperidone)
neuroleptics have a high affinity for D2
receptors.
241-4.63
66
Pharmacotherapy for DrugAbuse Relapse Prevention
Drug Natrexone (Trexan) opioid and alcohol
dependency Disulfiram (Antabuse) alcohol
dependency Clonidine (Catapres) opioid
withdrawal Methadone (Dolophine) opioid
dependency Buprenorphine (Buprenex) opioid
dependency Nicotine patches and
gum Ibogaine (Endabuse) - anticraving
Acamprosate anti-alcohol craving Immunization
(experimental animals) - Morphine - Cocaine
241-4.64
67
Modification of Behavior After Withdrawal
Psychotherapy Little evidence that traditional
individual psychotherapy is of value for
compulsive drug user. Cognitive or expressive
psychotherapy has improved poor prognosis
patients in methadone programs. Special forms
of group therapy and self-help groups have been
demonstrated to reduce relapse. Voluntary Groups
and Self-Regulatory Communities Alcoholic
anonymous, narcotics anonymous, Phoenix House,
etc. Supervised-Deterrent Approaches
Abstinence during a period in a hospital, prison,
or special facility followed by supervision in
the community.
241-4.65