Case 1 SF - PowerPoint PPT Presentation
Title:
Case 1 SF
Description:
Case 1 SF 41 y/o woman with no PMHx p/w blurry vision and headache worsening x few weeks. No meds, no toxic habits. PE: Afeb VSS. Bilateral lid swelling. – PowerPoint PPT presentation
Number of Views:117
Avg rating:3.0/5.0
Title: Case 1 SF
1
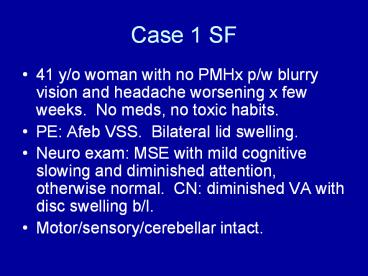
Case 1 SF
- 41 y/o woman with no PMHx p/w blurry vision and
headache worsening x few weeks. No meds, no
toxic habits. - PE Afeb VSS. Bilateral lid swelling.
- Neuro exam MSE with mild cognitive slowing and
diminished attention, otherwise normal. CN
diminished VA with disc swelling b/l. - Motor/sensory/cerebellar intact.
2
(No Transcript)
3
Other w/u
- LP elevated opening pressure, CSF lymphocytic
pleocytosis (60-80), prt 80 - Serum ACE 65
- CSF ACE 20
4
(No Transcript)
5
Clinical course
- Progressive cognitive decline, recurring bouts of
aseptic meningitis with visual blurring partially
responsive to IV steroids. - Poor compliance? pulse Cytoxan
- Later developed poor vision d/t glaucoma and b/l
optic neuritis - Panhypopituitarism
- Dementia
6
Case 2 RC
- 44 y/o man with hx of CVA and behavioral
problems, p/w AMS and difficulty walking. Prior
CVA admitted at Montefiore 2005, p/w . W/u
revealed basal ganglia and cerebellar
calcification on CT scan, acute R
midbrain/thalamic infarct on MRI. Cause of
stroke in young uncertain, however pt found to be
ANA. - Meds
7
- PE Afeb VSS
- Neuro MSE alert, Ox2, dim attention, STM 1/3.
- CN dysarthric, otherwise intact
- Motor increased tone in legs, full strength,
mild incoordination on FTN, - DTRs hyperactive
- Gait spastic/ataxic
8
Imaging
9
Other w/u
- ESR 120
- Creatinine 2-3 (prior baseline 1-1.5)
- ANA and dsDNA
- Anti-cardiolipin Ab
- MRI spinal cord no significant abnl
- Cerebral angiogram possibly slight medium vessel
irregularity c/w vasculopathy
10
Clinical course
- IV steroids
- IVIG
- Mycophenolate
- Warfarin
- Worsening dementia and paraparesis
- D/c to SNF
11
CNS Inflammatory Disease
- Primary, recurrent demyelinating diseases MS,
Neuromyelitis Optica (NMO, Devics Dx) - Mono-phasic demyelinating diseases Acute
disseminated encephalomyelitis (ADEM), acute
hemorrhagic leukoencephalitis (AHLE), transverse
myelitis (TM), optic neuritis (ON) often these
are para-infectious - CNS involvement with systemic (clinical or
sub-clinical) auto-immune disease includes
primary and secondary CNS vasculitis - Paraneoplastic dx
- Immune reconstitution inflammatory syndrome
(IRIS) - CNS infections (discussed in other lecture)
12
Systemic inflammatory conditions with frequent
neurological manifestations
- SLE neuropsychiatric manifestations
- Sjogrens
- Sarcoid
- Anti-phospholipid Ab syndrome (1º or 2º)
- Rheumatoid arthritis PNS
- Vasculitis large or small vessel
- Large Giant cell arteritis CNgtCVA
- Small Wegeners, polyarteritis nodosum
mononeuritis multiplex gt CN gtgtCNS - Paraneoplastic syndromes cerebellar dx, limbic
encephalitis, PNS
13
Focal Clinical Presentation
- Focal CNS deficit (brain or brainstem)
hemiparesis, hemisensory loss, hemiataxia,
diplopia, vertigo, dysarthria - Spinal cord syndrome complete (motor/sensory/auto
nomic), anterior, posterior, Brown Sequard - Cranial nerve optic neuritis, trigeminal
neuralgia, facial paresis - Pseudo-peripheral Lhermittes sign,
paresthesias, pain - Focal cognitive deficit aphasia, apraxia, neglect
14
Neuropyschiatric SLE 19 syndromes described
Joseph (2007) Neurology
15
(No Transcript)
16
NPSLE
- Neurological dx present in 50 (15-90)
- Presenting with neuro symptoms 3-5
- NPSLE worsens prognosis
- NPSLE can occur without systemic flare
- Lab abnl ESR elevated 50, ANA 85, dsDNA 72,
anti-phospholipid Ab 30, complement low during
flare 44, ribosomal P Ab and C3A frequently
elevated prior to/during flare. - APS associated with NPSLE, CVA, other focal dx
17
Neuro testing in NPSLE
- CSF abnl 20-40 (lymphocytic pleocytosis,
elevated prt, OCB each present in 20). - EEG abnl up to 80 abnl, mostly non-specific
changes but some with epileptogenic focus. - EMG/NCS high abnl in symptomatic PNS dx
18
Neuroimaging
- Brain MRI abnl in 20-70 most common findings
are multifocal small white matter
hyperintensities and atrophy stroke in lt 20
lower show basal ganglia calcification,
reversible leukoencephalopathy syndrome (RPLS). - SPECT detects multifocal or patchy/diffuse
perfusion deficits in 50-90 - MR spectroscopy abnl in ? 20-50
19
MRI abnl in NPSLE ptsCsepany (2003) J Neurol
20
NPSLE RxSanna 2003
21
CNS LupusCsepany 2003
22
Lupus RPLSMagnano 2006
23
EMT with SLE, APS, complicated migraine with
aphasia and RHP
24
Neurosarcoidosis
- Neurological manifestations in 10 (20 at
autopsy). - Rarely presents with neurologic syndrome
- Very rarely limited to NS
25
Joseph (2008) JNNP
26
(No Transcript)
27
Spencer (2004) Sem Arthritis Rheum
28
(No Transcript)
29
Laboratory findings in neurosarcoidosis
- CXR abnl 40-50 (30-80 range)
- Chest CT abnl 60-75 (? up to 90)
- Gallium/PET scan abnl 25-80
- Serum ACE elevation 25-75
- CSF prt elevation 50
- CSF lymphocytic pleocytosis 40
- CSF OCB 20-40
30
Neurosarcoid MRI abnl
- Any abnl up to 80
- Leptomeningeal or parenchymal enhancement 25-50
- White matter lesions 30-50
31
Neurological manifestations of Sjogrens syndrome
- Common disorder, affecting 2-3 of adults.
- Neurological dx present in 5-60.
- CNS and PNS dx both common.
- Neurological symptoms occur prior to diagnosis in
80-90 of patients. - Sicca symptoms present in lt50 at presentation.
32
(No Transcript)
33
(No Transcript)
34
PNS SjogrensMori (2005) Brain
35
MRI, path, and sweat testing in Sjogrens sensory
neuropathy (Mori 2005)
36
Lab abnl in Neuro-Sjogrens
- SSA/SSB 45
- Schirmers test abnl 90
- Salivary scintography abnl 65
- Lip bx abnl 95
37
References
- SLE
- Joseph (2008) JNNP
- Sanna (2003) Lupus
- Csepany et al (2003) J Neurol
- Sjogrens
- Mori (2005) Brain
- Delalande (2004) Medicine
- Soliotis (1999) Ann Rheum Dis
- Sarcoid
- Joseph (2008) JNNP
- Joseph (2007) Practical neurology
- Spencer (2004) Sem Arthritis Rheum
38
NeurosarcoidSpenser 2004
39
CNS Sjogrens