Client%20with%20gout - PowerPoint PPT Presentation
Title:
Client%20with%20gout
Description:
Client with gout Definition a. Syndrome occurs from inflammatory response to production or excretion of uric acid resulting in high levels of uric acid in blood and ... – PowerPoint PPT presentation
Number of Views:171
Avg rating:3.0/5.0
Title: Client%20with%20gout
1
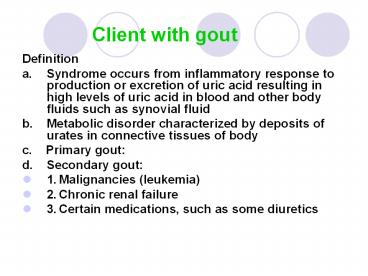
Client with gout
- Definition
- a. Syndrome occurs from inflammatory response to
production or excretion of uric acid resulting in
high levels of uric acid in blood and other body
fluids such as synovial fluid - b. Metabolic disorder characterized by deposits
of urates in connective tissues of body - c. Primary gout
- d. Secondary gout
- 1. Malignancies (leukemia)
- 2. Chronic renal failure
- 3. Certain medications, such as some diuretics
2
Client with gout
- Pathophysiology
- a. Uric acid is a breakdown product of purine
metabolism and is normally excreted through urine
and feces - b. Levels gt 7.0 mg/dL (normal 3.4 7.0 mg/dL in
males 2.4 6.0 mg/dL in females) lead to
formation of urate crystals in peripheral tissues
(synovial membranes, cartilage, heart, earlobe,
kidneys) and perpetuate inflammation
3
Client with gout
- Manifestations 3 stages in untreated gout
- a. Hyperuricemia
- 1. Uric acid levels average 9 10 mg/dL
- 2. Recurrent attacks of inflammation of single
joint - 3. Tophi in and around the joint
- 4. Renal disease and renal stones
- 5. Many persons do not progress beyond this level
- b. Acute gouty arthritis
- 1. Acute attack usually affecting a single joint
- 2. May be triggered by trauma, alcohol ingestion,
dietary excess, stressor, such as surgery or
hospitalization - 3. Affected joint is red, hot, swollen, very
painful and tender often first
metatarsophalangeal joint (great toe) - 4. Accompanied by fever, elevated WBC and ESR
- 5. Episode last hours to weeks followed by
asymptomatic period
4
Client with gout
- Tophaceous (chronic) gout
- 1. Occurs when hyperuricemia not treated
- 2. Tophi develop in cartilage, synovial
membranes, tendons, soft tissues - 3. Skin over tophi may ulcerate exude chalky
material and urate crystals - 4. Leads to joint deformities and nerve
compression - 5. May lead to kidney disease (uric acid stones
and can lead to ARF) - Collaborative Care
- a. Treatment directed towards ending acute attack
- b. Treatment directed towards preventing
recurrent attacks and complications
5
Client with gout
- Diagnostic Tests
- a. Diagnosis with classic presentation by
history and physical examination - b. Uric acid
- c. WBC
- d. Erythrocyte sedimentation rate (ESR) elevated
from acute inflammation process - e. 24-hour urine collection to determine uric
acid production and excretion - f. Fluid aspirated from acutely inflamed joints
shows urate crystals
6
Client with gout
- Medications
- a. Used to terminate acute attack and prevent
future ones - b. Reduce serum uric acid levels
- c. Treatment of acute gout attack
- 1. NSAIDs, specifically indomethacin (Indocin)
- 2. Colchicine interrupts cycle of urate crystal
deposits and inflammation - a. Anti-inflammatory use limited to gout
- b .Use limited by significant side effects with
oral administration abdominal cramping,
diarrhea, nausea, vomiting - 3. Corticosteroids, including intra-articular
route - 4. Analgesia, including narcotics
7
Client with gout
- Prophylactic therapy
- 1. Clients who do not eliminate uric acid
adequately are treated with colchicines and
uricosuric drugs, such as probenecid (Benemid)
and sulfinpyrazone (Aprazone, Anturane, Zynol) - 2. Clients who produce excessive amounts of uric
acid are treated with allopurinol (Zyloprim),
which lowers serum uric acid levels
8
Client with gout
- Dietary Management
- a. Dietary purines contribute only slightly to
uric acid levels if low-purine diet recommended,
client must avoid all meats, seafood, yeast,
beans, oatmeal, spinach, mushrooms - b. Client may be advised to lose weight, but
fasting not advised - c. Avoid alcohol, foods known to precipitate gout
attack - Other Treatments
- a. During acute attack of gouty arthritis, bed
rest until 24 hours post attack, elevate joint
with hot or cold compresses - b. Liberal fluid intake (2000 mL) to increase
urate excretion urinary alkalinizing agents
(sodium bicarbonate and potassium citrate) to
minimize risk of uric acid stones
9
Client with gout
- Nursing Diagnoses
- a. Acute Pain
- b. Impaired Physical Mobility
- Home Care
- a. Education regarding prescribed medications
- b. Education on maintaining high fluid intake of
fluid and avoiding alcohol
10
Client with osteoarthritis (OA)
- Description
- a. Most common of all forms of arthritis
- b. Characterized by loss of articular cartilage
in articulating joints and hypertrophy of bones
at articular margins - c. Causes are idiopathic or secondary (post
injury) - d. Affects more than 60 million adult Americans
- e. Males more often than females, until age 55
when incidence twice as high in females - f. Men more likely to have OA in the hips, women
in the hands
11
Client with osteoarthritis (OA)
- Risk Factors
- a. Age, but may be inherited as autosomal
recessive trait - b. Excessive weight especially in hip and knee
- c. Inactivity
- d. Strenuous, repetitive exercise as with sports
participants increased risk for secondary OA - e. Hormonal factors such as decreased estrogen in
menopausal women
12
Client with osteoarthritis (OA)
- Pathophysiology
- a. Cartilage lining joints degenerates and loses
tensile strength loss of articular cartilage
results in bone thickening, reducing the ability
to absorb energy in joint loading - b. Osteophytes (bony outgrowths) form, change
anatomy of joint these spurs enlarge, break off
and lead to mild synovitis
13
Joint changes in degenerative joint disease
14
Client with osteoarthritis (OA)
- Manifestations
- a. Onset is gradual, insidious, slowly
progressive - b. Pain and stiffness in one or more joints pain
is a deep ache aggravated by use of motion and
relieved by rest but may be persistent with time - c. Pain may be referred to other places
- d. Periods of immobility are followed by
stiffness - e. Decreased range of motion of joint and grating
or crepitus during movement - f. Bony overgrowth causes joint enlargement
- 1. Herberdens nodes terminal, interphalangeal
joints - 2. Bouchards nodes proximal, interphalangeal
joints - g. Flexion contractures occur with joint
instability
15
Client with osteoarthritis (OA)
- Complications Spondylosis, a degenerative disk
disease, which may lead to herniated disk - Collaborative Care
- a. Relieve pain
- b. Maintain clients function and mobility
- Diagnostic Tests
- a. Based on clients history and physical
examination - b. Characteristic changes seen on xray
16
Client with osteoarthritis (OA)
- Medications
- a. Pain management with aspirin, acetaminophen,
NSAIDs - b. Capsaicin cream topically to reduce joint pain
and tenderness - c. NSAID COX-2 inhibitors
- 1. Results similar to conventional NSAIDs with
fewer GI and renal systems side effects - 2. Meloxicam (Mobic), celecoxib (Celebrex),
rofecoxib (Vioxx) - d. Corticosteroid injection of joints, but this
may hasten rate of cartilage breakdown
17
Client with osteoarthritis (OA)
- Conservative Treatment
- a. Physical therapy
- b. Rest of involved joint
- c. Using ambulation devices
- d. Weight loss
- e. Analgesic and anti-inflammatory medications
18
Client with osteoarthritis (OA)
- Surgery
- a. Arthroscopy
- 1. Arthroscopic debridement and lavage of
involved joints - 2. Unclear about effectiveness long term
- b. Osteotomy
- 1. Incision into or transection of bone to
realign affected joint - 2. Shifts joint load toward areas of less
cartilage damage - 3. Delays joint replacement for several years
- c. Joint arthroplasty
- 1. Reconstruction or replacement of joint
indicated when client has severely restricted
joint mobility and pain at rest - 2. Total joint replacement is procedure done for
most OA clients, which involves replacing both
surfaces of affected joint with prosthetic parts
19
Client with osteoarthritis (OA)
- Complementary Therapies
- a. Bioelectromagnetic therapy
- b. Elimination of nightshade foods
- c. Nutritional supplements, herbal therapies,
vitamins - d. Osteopathic manipulation
- e. Yoga
- Nursing Care
- a. Promote comfort
- b. Maintain mobility
- c. Assist with adaptation of life style
20
Client with osteoarthritis (OA)
- Health Promotion
- a. Maintenance of normal weight
- b. Program of regular, moderate exercise
- c. Use of glucosamine and chrondroitin
- Nursing Diagnoses
- a. Chronic Pain
- b. Impaired Physical Mobility
- c. Self-care Deficit
- Home Care
- a. Education regarding avoiding overuse or stress
on affected joints - b. Education regarding pharmacological and other
forms of pain-relief - c. Clients post TJR activity restrictions and
assistive devices
21
Rheumatoid arthritis (RA)
- Definition
- a. Chronic systemic autoimmune disease causing
inflammation of connective tissue primarily in
joints - 1. Three times more likely to affect females than
males - 2. Onset is between 20 40 years
- b. Course and severity are variable clients
exhibit pattern of symmetrical multiple
peripheral joints involvement with periods of
remission and exacerbation - c. Cause is unknown combination of genetic,
environmental, hormonal, reproductive factors
infectious agents, especially Epstein-Barr,
thought to play role
22
Rheumatoid arthritis (RA)
- Pathophysiology
- a. Normal antibodies become autoantibodies
(rheumatoid factors -RF) and attack host tissues,
which bind with target antigens in blood and with
synovial membranes forming immune complexes - b. Synovial membrane damaged from inflammatory
and immune processes leads to erosion of
articular cartilage and inflammation of ligaments
and tendons - c. Granulation tissue (pannus) forms over denuded
areas of synovial membrane and scar tissue forms
immobilizing joint
23
Rheumatoid arthritis (RA)
- Joint manifestations
- a. Onset is usually insidious but may be acute
after stressor, such as infection - b. Systemic manifestations fatigue, anorexia,
weight loss and non-specific aching and stiffness
precedes joint involvement - c. Joint swelling with stiffness, warmth,
tenderness and pain usually multiple joints and
symmetric involvement - d. Proximal interphalangeal and
metacarpophalangeal joints of fingers, wrists,
knees, ankles, and toes are frequently involved - e. Joint deformity of fingers include swan-neck
deformity and boutonniere deformity wrist
deformity leads to carpel tunnel syndrome knee
deformity leads to disability and feet and toes
develop typical deformities
24
Joint destruction in rheumatoid arthritis
25
Rheumatoid arthritis (RA)
- Extra-articular manifestations
- a. While disease is active fatigue, weakness,
anorexia, weight loss, low-grade fever - b. Anemia develops as does skeletal muscle
atrophy - c. Rheumatoid nodules develop in subcutaneous
tissue in areas subject to pressure on forearm,
olecranon bursa, over metacarpophalangeal joints - d. Pleural effusion, pericarditis, splenomegaly
may occur
26
Rheumatoid arthritis (RA)
- Collaborative Care
- a. Relief of pain and reduction of inflammation
- b. Slow or stop joint damage
- c. Improve well-being and ability to function
- d. Relief of manifestations
27
Rheumatoid arthritis (RA)
- Diagnostic Tests
- a. Client history and physical assessment
- b. Rheumatoid factors (RF), autoantibodies to IgG
present in 75 of persons with RA - c. Elevation of ESR indicator of disease and
inflammatory activity used to evaluate
effectiveness of treatment - d. Examination of synovial fluid signs
associated with inflammation - e. Xrays of affected joints show diagnostic
changes - f. CBC shows moderate anemia with elevated
platelet count
28
Rheumatoid arthritis (RA)
- Medications
- a. Aspirin and NSAIDs, mild analgesics to relieve
manifestations, but have little effect on disease
progression - 1. Aspirin
- a. Often first prescribed in high doses just
under toxic dose, which produces tinnitus and
hearing loss - b. GI side effects and interference with platelet
function are hazards associated with aspirin
therapy - c. May use enteric-coated forms of aspirin or
nonacetylated salicylate compounds
29
Rheumatoid arthritis (RA)
- NSAIDs
- a. Different, specific NSAIDs are tried to
determine the most effective drug for individual
clients - b. Have GI side effects and can be toxic to
kidneys - b. Low dose oral corticosteroids
- 1. To reduce pain and inflammation
- 2. To slow development and progression of disease
- 3. Often have dramatic effects, but long-term use
results in multiple side effects
30
Rheumatoid arthritis (RA)
- Treatments
- a. Balanced program of rest and exercise
- 1. Rest with exacerbation and may utilize
splinting - 2. Exercise to maintain ROM, muscle strength
- 3. Low impact exercise such as swimming or
walking - b. Physical and occupational therapy
- c. Heat and cold analgesia and muscle-relaxation
- d. Assistive devices and splints which help rest
joints and prevent contractures - e. Diet well-balanced some benefit from omega-3
fatty acids found in fish oils - f. Surgery variety of procedures may be done
synovectomy, arthrodesis, joint fusion,
arthroplasty or total joint replacement
31
Rheumatoid arthritis (RA)
- Nursing Care assist client to deal effectively
with physical manifestations and psychosocial
effects - Health Promotion
- a. Support client in becoming arthritis
self-managers prevent deformities and effects of
arthritis by balance of exercise and rest, weight
management, posture, and positioning - b. Referral Arthritis Foundation
- Nursing Diagnoses
- a. Chronic Pain increasing pain requires need to
decrease activity level - b. Fatigue
- c. Ineffective Role Performance
- d. Disturbed Body Image
- Home Care support for client and family to
become active in disease management
32
Systemic Lupus Erythematosus (SLE)
- Definition
- a. SLE is chronic inflammatory immune complex
connective tissue disease affecting multiple body
systems can range from mild episodic disorder to
rapidly fatal disease process - b. Affects mostly females in childbearing age
more common in African Americans, Hispanics,
Asians - c. Cause is unknown causative factors are
genetic, environmental, and hormonal - d. Most clients have mild chronic case with
periods of remissions and exacerbations those
with virulent disease often develop renal and CNS
involvement and death is related to infection
33
Systemic Lupus Erythematosus (SLE)
- Definition
- a. SLE is chronic inflammatory immune complex
connective tissue disease affecting multiple body
systems can range from mild episodic disorder to
rapidly fatal disease process - b. Affects mostly females in childbearing age
more common in African Americans, Hispanics,
Asians - c. Cause is unknown causative factors are
genetic, environmental, and hormonal - d. Most clients have mild chronic case with
periods of remissions and exacerbations those
with virulent disease often develop renal and CNS
involvement and death is related to infection
34
Systemic Lupus Erythematosus (SLE)
- Pathophysiology
- a. Production of large variety of autoantibodies
against the normal components of body especially
the nucleic acids leads to development of immune
complexes which leads to tissue damage in
multiple organs - b. Reaction to some medications (procainamide,
hydralazine) causes a syndrome similar to lupus,
which usually resolves when medication is
discontinued
35
Systemic Lupus Erythematosus (SLE)
- Manifestations
- a. Early manifestations fever, anorexia,
malaise, weight loss, multiple arthralgias and
symmetric non-deforming polyarthritis - b. Skin manifestations usually occur red
butterfly rash across the cheeks and bridge of
the nose accompanied by photosensitivity
(maculopapular rash upon sun exposure) alopecia
is common - c. 50 of persons have renal involvement
including proteinuria, cellular casts, and
nephrotic syndrome 10 develop renal failure - d. Hematologic manifestations
- e. Cardiovascular system
- f. Pulmonary system
- g. Neurologic involvement
- h. Ocular system
- i. GI symptoms
36
Systemic Lupus Erythematosus (SLE)
- Collaborative Care
- a. Diagnosis is often difficult due to the
diversity of manifestations in individual clients - b. Effective management has improved survival rate
37
Systemic Lupus Erythematosus (SLE)
- Diagnostic Tests
- a. Clinical history, physical examination
- b. Anti-DNA of various antibodies, this antibody
is more specific for SLE rarely found in any
other disorder - c. ESR typically elevated, especially during
exacerbations - d. Serum complement levels levels are low (used
in development of antigen-antibody complexes) - e. CBC severe anemia, leucopenia with
lymphcytopenia, thrombocytopenia - f. Urinalysis mild proteinuria, hematuria, blood
cell casts - g. BUN and creatinine determine renal function
- h. Kidney biopsy obtain accurate diagnosis of
kidney lesion and plan definitive treatment with
renal insufficiency
38
Systemic Lupus Erythematosus (SLE)
- Medications
- a. Mild cases of SLE may be treated with
supportive care and possible aspirin and NSAIDs - b. Skin and arthritic manifestations are treated
with anti-malarial drugs - c. Severe cases are often treated with high-dose
corticosteroid therapy tapered as clients
disease allows treatment may also include
immunosuppressive agents (cyclophosphamide or
azathioprine) alone or with the steroids
39
Systemic Lupus Erythematosus (SLE)
- Other treatments
- a. Avoid sun exposure use of sunscreens
- b. Clients with ESRD require dialysis and kidney
transplantation - Nursing Care client with severe disease has
needs related to system involvement and similar
to client with RA
40
Systemic Lupus Erythematosus (SLE)
- Nursing Diagnoses
- a. Impaired Skin Integrity
- b. Ineffective Protection
- 1. Teach client to follow aseptic techniques
- 2. Monitor closely for signs of infection, which
are often suppressed - c. Impaired Health Maintenance client often has
involved physical and psychological needs - Home Care
- a. Teaching regarding skin care, avoiding sun,
following treatment plan including medications - b. Wearing medical identification
- c. Family planning
- d. Referral to home nursing care, resources and
support groups