Immunology 01:146:474 PowerPoint PPT Presentation
1 / 36
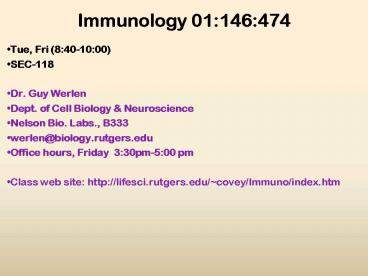
Title: Immunology 01:146:474
1
Immunology 01146474
- Tue, Fri (840-1000)
- SEC-118
- Dr. Guy Werlen
- Dept. of Cell Biology Neuroscience
- Nelson Bio. Labs., B333
- werlen_at_biology.rutgers.edu
- Office hours, Friday 330pm-500 pm
- Class web site http//lifesci.rutgers.edu/covey/
Immuno/index.htm
2
Charles A. Janeway, Paul Travers, Mark Walport,
Mark Shlomchik
Immunobiology The Immune System in Health
DiseaseSixth Edition
Failure of host defense mechanisms Chapter 11
- Pathogens have evolved various means of evading
or subverting normal host defenses - Immunodeficiency syndrome
- Acquired immune deficiency syndrome (AIDS)
3
Immunodeficiency diseases
4
Defects in phagocytic cells permit widespread
bacterial infections
5
Defects in phagocytic cells leads to persistent
bacterial infections
6
Defects in complement component cause defective
humoral immune function
7
Defects in complement component are associated
with susceptibility to bacterial infections and
accumulation of immune complexes
8
Defects in thymus structure or thymocyte homing,
blocks T cell development and induces severe
immunodeficiency
9
The nude mouse strain is athymic due to a
mutation in the Foxn1nu gene that encodes FOXN1,
a transcription factor of the forkhead box
family. FOXN1 is preferentially expressed in the
skin and thymus. Alteration of its expression in
the thymus underlies the manifestation of severe
Immunodeficiency resulting from total absence of
T cell development.
10
Generation of a KO mouse models by targeted gene
disruption have been instrumental in
understanding the immune system and its defects
11
?2m is part of MHC Class I molecules and it is
required for effective antigen presentation
during thymocyte development
?2m
12
Defects in antigen presentation induces selective
Immunodeficiency of the corresponding MHC
class-restricted T cells
13
Distinct mutations in the VDJ gene recombination
or DNA repair machinery cause severe combined
immunodeficiency syndromes
14
- Distinct mutations in the gene recombination
- machinery cause SCID syndromes
- Rag-1, Rag-2 gene Omenns syndrome
- DNA-PKc gene scid
- DNA helicase Blooms syndrome
- ATM kinase ataxia telangiectasia
15
Defects in purine degradation leads to major
combined immunodeficiency syndromes due to the
accumulation of nucleotide metabolites that are
toxic for developing T and B cells
Defects in the purine degrading enzymes
adenosine deaminase (ADA) or purine
phos- phorylase (PNP) totally block lymphoid cell
development
16
Defects in T cell development or activation lead
to major immunodeficiency syndromes that
underline the critical regulatory role of T
cells in the immune system
17
Defect in cytokine production or action can
cause immunodeficiency
A defect in the ?c receptor causes X-linked
severe combined immunodeficiency X-linked SCID
IL-7 is critical for thymocyte development. IL-2
is critical for naïve T cell proliferation. IL-4
is critical for Th2 cell differentiation and
proliferation. IL-9 Th2 cell activator. Il-15 T
growth factor.
18
Defects in T cell signaling block T cell
development and result in severe combined
immunodeficiency.
Deficiency in antigen presentation
(MHC) TCR/CD3 expression (TCR?
CD3?) proximal tyrosine kinase (ZAP-70) result
in an arrest of T cell development at the CD4CD8
DP thymocyte stage.
19
Bone marrow transplantation or gene therapy can
be useful to correct genetic defects of the
immune system.
Bone marrow donor and recipient must share at
least some MHC molecules to restore immune
function
Shared MHC of type b (blue). Unshared donor MHC
of type a (yellow).
20
But an immune reaction against the graft must be
avoided or controlled to prevent a graft
rejection
Graft-versus-host disease Mature T cells from
graft attack cells of the host.
Host-versus-graft response Competent T cells of
the host can attack the donor bone marrow stem
cells
T cell depletion of the donor bone marrow
prevents graft- versus-host disease.
21
Acquired immune deficiency syndrome (AIDS)
a disease without borders
22
HIV is a RNA retrovirus of the lentivirus family
that infects mainly CD4 T cells
Macrophage-tropic HIV variant bind to CCR5 on
macrophages DC, CD4 T cells
Lymphocyte-tropic HIV variant bind only to CXCR4
on activated CD4 T cells
23
Dendritic cells initiate HIV infection by
transporting the virus from mucosal surfaces to
lymphoid tissues
- - Gp120 of R5 HIV variants binds to DC-SIGN of
intraepithelial dendritic - cells layering the mucosal surface of the sexual
and excretory organs. - In addition, gp120 of R5 HIV can also bind to
CCR5 expressed on the - epithelial cells of the mucosa in the intestinal
tract, including rectum - endocervix. HIV translocates from infected
epithelial cells to sub- - mucosal CD4 T cells and dendritic cells
24
HIV infection due to blood transfusion
HIV infection propagates via exchange of body
fluids such as infected blood transfusions that
replace clotting factor VIII, a coagulation
component that is defective in hemophiliac
patients. Age is a factor in the progression to
AIDS.
25
The gp120 of HIV binds with high affinity to CD4
on the surface of T cells that recirculate
through the lymphoid tissues
26
The viral genome is integrated into the host DNA
27
The RNA genome of HIV is flanked by long terminal
repeats and essentially contains genes that code
for capsid and infectivity proteins
28
Activation of CD4 T cells is required to induce
the transcription of the HIV provirus
29
Structural proteins of HIV are synthesized and
new capsids are formed
30
HIV infection is long lasting and induces
specific CD4 T cell immunodeficiency.
HIV infection induces an acute flu-like disease
characterized by a rapid loss of CD4 T cells.
Follows an adaptive immune response that controls
the acute illness and partially restores the
level of CD4 T cells in the blood. The adaptive
immune response does not eradicate HIV.
Repetitive opportunistic infections contribute
to tear and wear of the immune system and a
continuous depletion of CD4 T cells from the
blood.
31
While the immune response mounts a specific
response against HIV, it is not successful and
declines over time
Even though high HIV antibody titers and CTL
responses are observed during the asymptomatic
phase, this concerted immune response is not
sufficient to avoid persistent HIV replication in
CD4 T cells. Eventually, antibody titers and CTL
responses decline, while HIV replication
increases (symptomatic phase). This leads to a
terminally ill AIDS phase during which the immune
system is completely overwhelmed.
32
HIV induces an immunodeficiency, which leads to
persistent infections by opportunistic pathogens
Respiratory infections (Pneumocystis
mycobacterium) are the major cause of death of
AIDS patients.
33
HIV resistance to protease inhibitors is the
challenge for new drug development
The first generation of HIV inhibitors
specifically blocked the endogenous protease of
the virus. However after a rapid decline in viral
titer and a synergistic recovery of CD4 T cell
counts, the high mutation rate of HIV creates
resistance to the drug with a new infection
cycle.
34
Effect of combined drug therapies on the
morbidity and mortality of HIV infection in the
USA
The use of drug combination (protease inhibitors
and viral reverse-transcriptase inhibitors)
effectively decreases opportunistic infections
and death of HIV infected patients.
35
Combined drug treatment successfully decreases
HIV titer, But they do not completly cure the
infection
The combination of protease inhibitors and viral
reverse- transcriptase inhibitors blocks the
production of new HIV particles for a prolonged
time. First phase viral production declines
sharply due to death of CD4 T cells that were
productively infected with HIV prior to
treatment. Second phase HIV is released from
Mø and from resting latently, infected CD4 T
cells that are then stimulated to divide and
that develop productive HIV infection. Third
phase of undetermined length reactivation of
integrated provirus in memory T cells and other
long-lived reservoir of infection
36
Prevention Better education Elementary Hygiene