Code of Ethics PowerPoint PPT Presentation
1 / 60
Title: Code of Ethics
1
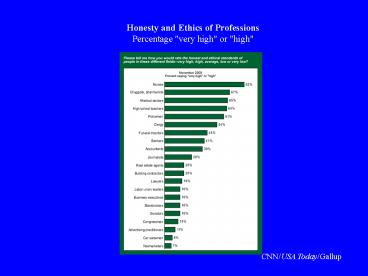
Honesty and Ethics of ProfessionsPercentage
"very high" or "high"
CNN/USA Today/Gallup
2
Code of Ethics
- Ethics vs. Laws
- Is a code of ethics necessary?
- Does a code of ethics guide professional
behavior? - Is being a good person enough?
- What would our profession be like without ethical
practitioners?
3
Why Regulate Healthcare?
- Laws exist because a purely market-driven system
fails to protect the public health, safety, and
welfare. - Incentive to maximize profit can compromise and
conflict with the best interest of
patients/customers. - The race to the bottom
4
Why have a Code of Ethics?
- The code is to protect each professional from
certain pressures (for example, the pressure to
cut corners to save money) by making it
reasonably likely...that most other members of
the profession will not take advantage of her
good conduct. A code protects members of a
profession from certain consequences of
competition. A code is a solution to a
coordination problem.
Michael Davis Senior Research Associate at the
Center for the Study of Ethics in Professions,
Illinois Institute of Technology
5
Business vs. Profession
- Is Pharmacy a business or a profession? Both?
- Differences between business and profession?
- Are there business/political ethics?
- Enron, Global Crossing, Adelphia, Martha Stewart,
Jack Abramoff
6
American Medical Association
- Principles of Medical Ethics
- A physician shall be dedicated to providing
competent medical care, with compassion and
respect for human dignity and rights. - A physician shall uphold the standards of
professionalism, be honest in all professional
interactions, and strive to report physicians
deficient in character or competence, or engaging
in fraud or deception, to appropriate entities. - A physician shall respect the law and also
recognize a responsibility to seek changes in
those requirements which are contrary to the best
interests of the patient. - A physician shall respect the rights of patients,
colleagues, and other health professionals, and
shall safeguard patient confidences and privacy
within the constraints of the law.
7
American Medical Association
- A physician shall continue to study, apply, and
advance scientific knowledge, maintain a
commitment to medical education, make relevant
information available to patients, colleagues,
and the public, obtain consultation, and use the
talents of other health professionals when
indicated. - A physician shall, in the provision of
appropriate patient care, except in emergencies,
be free to choose whom to serve, with whom to
associate, and the environment in which to
provide medical care. - A physician shall recognize a responsibility to
participate in activities contributing to the
improvement of the community and the betterment
of public health. - A physician shall, while caring for a patient,
regard responsibility to the patient as
paramount. - A physician shall support access to medical care
for all people. - Adopted by the AMA's House of Delegates June
17, 2001
8
Pharmacist Code of Ethics
- Adopted by APhA in 1994
- Endorsed by ASHP in 1996
- Actually read by very few practicing pharmacists!
9
Code of Ethics for Pharmacists
PREAMBLE Pharmacists are health professionals who
assist individuals in making the best use of
medications. This Code, prepared and supported
by pharmacists, is intended to state publicly the
principles that form the fundamental basis of the
roles and responsibilities of pharmacists. These
principles, based on moral obligations and
virtues, are established to guide pharmacists in
relationships with patients, health
professionals, and society.
10
Code of Ethics for Pharmacists
I. A pharmacist respects the covenantal
relationship between the patient and
pharmacist. Considering the patient-pharmacist
relationship as a covenant means that a
pharmacist has moral obligations in response to
the gift of trust received from society. In
return for this gift, a pharmacist promises to
help individuals achieve optimum benefit from
their medications, to be committed to their
welfare, and to maintain their trust.
11
Code of Ethics for Pharmacists
II. A pharmacist promotes the good of every
patient in a caring, compassionate, and
confidential manner. A pharmacist places
concern for the well-being of the patient at the
center of professional practice. In doing so, a
pharmacist considers needs stated by the patient
as well as those defined by health science. A
pharmacist is dedicated to protecting the dignity
of the patient. With a caring attitude and a
compassionate spirit, a pharmacist focuses on
serving the patient in a private and confidential
manner.
12
Code of Ethics for Pharmacists
III. A pharmacist respects the autonomy and
dignity of each patient. A pharmacist promotes
the right of self-determination and recognizes
individual self-worth by encouraging patients to
participate in decisions about their health. A
pharmacist communicates with patients in terms
that are understandable. In all cases, a
pharmacist respects personal and cultural
differences among patients.
13
Code of Ethics for Pharmacists
IV. A pharmacist acts with honesty and integrity
in professional relationships. A pharmacist
has a duty to tell the truth and to act with
conviction of conscience. A pharmacist avoids
discriminatory practices, behavior or work
conditions that impair professional judgment, and
actions that compromise dedication to the best
interests of patients.
14
Code of Ethics for Pharmacists
V. A pharmacist maintains professional
competence. A pharmacist has a duty to maintain
knowledge and abilities as new medications,
devices, and technologies become available and as
health information advances.
15
Code of Ethics for Pharmacists
VI. A pharmacist respects the values and
abilities of colleagues and other health
professionals. When appropriate, a pharmacist
asks for the consultation of colleagues or other
health professionals or refers the patient. A
pharmacist acknowledges that colleagues and other
health professionals may differ in the beliefs
and values they apply to the care of the patient.
16
Code of Ethics for Pharmacists
VII. A pharmacist serves individual, community,
and societal needs. The primary obligation of a
pharmacist is to individual patients. However,
the obligations of a pharmacist may at times
extend beyond the individual to the community and
society. In these situations, the pharmacist
recognizes the responsibilities that accompany
these obligations and acts accordingly.
17
Code of Ethics for Pharmacists
VIII. A pharmacist seeks justice in the
distribution of health resources. When health
resources are allocated, a pharmacist is fair and
equitable, balancing the needs of patients and
society.
18
APhA Conscience Clause
- Pharmacist Conscience Clause
- 1. APhA recognizes the individual pharmacists
right to exercise conscientious refusal and
supports the establishment of systems to ensure
patients access to legally prescribed therapy
without compromising the pharmacists right of
conscientious refusal. - 2. APhA shall appoint a council on an as needed
basis to serve as a resource for the profession
in addressing and understanding ethical issues.
19
Choices!
20
Choice
- Ethical decisions occur when choices are made
among all possible courses of action - Not all choices involve ethical issues
- When they do, how do we make decisions?
- Using ethical principals
- Respect for autonomy
- Nonmaleficence
- Beneficence
- Justice
21
Conflict of Interest
- Also called competing interests
- When an individual has an interest in two (or
more) conflicting responsibilities, desires,
goals, desired outcomes - Examples Physician ownership of medical
laboratories, pharmacies, or other services - Authorship of an editorial review for a drug made
by a company in which you own stock.
22
Hospital Ethics Committee
- Assists medical staff with difficult cases
- Makes policy recommendations
- Provides education to physicians hospital staff
- Members
- Physicians, chaplains, nurses, social workers,
public members
23
Veracity
- Comprehensive, accurate, and objective transfer
of information - Depends on obligation of respect for others
- Closely related to fidelity
- Essential for trusting relationship
24
Privacy
- A human right the Right to Privacy
- Informational privacy
- Personal information
- Physical privacy
- Personal space
- Decisional privacy
- Personal choices
- Proprietary privacy
- Property (e.g. tissue samples)
25
Confidentiality
- Keeping information from being known
- informational privacy
- Medical confidentiality occurs upon disclosure
from one person to another (usually patient to
doctor) - Information is private and imparted in confidence
and trust
26
Fidelity
- Act in good faith
- Keep vows and promises
- Fulfill agreements
- Maintain relationships
- Discharge fiduciary responsibilities (act in the
patients best interest)
27
Parental Consent/Disclosure
- ORS 109.640
- Right to medical or dental treatment without
parental consent physicians may provide birth
control information to any person - Any physician may provide birth control
information and services to any person without
regard to the age of such person and a minor 15
years of age or older, may give consent to
hospital care, medical or surgical diagnosis or
treatment by a physician licensed by the Board of
Medical Examiners for the State of Oregon, and
dental or surgical diagnosis or treatment by a
dentist licensed by the Oregon Board of
Dentistry, without the consent of a parent or
guardian, except as may be provided by ORS
109.660.
28
Parental Consent/Disclosure
- ORS 109.680
- Disclosure without minor's consent civil
immunity - A physician, psychologist, nurse practitioner,
licensed clinical social worker or community
mental health and developmental disabilities
program described in ORS 109.675 may advise the
parent or parents or legal guardian of any minor
described in ORS 109.675 of the diagnosis or
treatment whenever the disclosure is clinically
appropriate and will serve the best interests of
the minor's treatment because the minor's
condition has deteriorated or the risk of a
suicide attempt has become such that inpatient
treatment is necessary, or the minor's condition
requires detoxification in a residential or acute
care facility. If such disclosure is made, the
physician, psychologist, nurse practitioner,
licensed clinical social worker or community
mental health and developmental disabilities
program shall not be subject to any civil
liability for advising the parent, parents or
legal guardian without the consent of the minor.
29
Parental Consent/Disclosure
- ORS 109.610
- Right to treatment for venereal disease without
parental consent - (1) Notwithstanding any other provision of law, a
minor who may have come into contact with any
venereal disease may give consent to the
furnishing of hospital, medical or surgical care
related to the diagnosis or treatment of such
disease, if the disease or condition is one which
is required by law or regulation adopted pursuant
to law to be reported to the local or state
health officer or board. Such consent shall not
be subject to disaffirmance because of minority. - (2) The consent of the parent, parents, or legal
guardian of such minor shall not be necessary to
authorize such hospital, medical or surgical care
and without having given consent the parent,
parents, or legal guardian shall not be liable
for payment for any such care rendered.
30
Death With Dignity Act 2004 Report
31
(No Transcript)
32
(No Transcript)
33
(No Transcript)
34
(No Transcript)
35
(No Transcript)
36
ETHICS CASES/EXAMPLES
37
Suspected Impairment
- You are an intern in a hospital pharmacy .
- You notice that the pharmacist you work with in
the IV Room frequently comes to work with an odor
of alcohol on his breath. - You report your suspicions to the pharmacy
manager, who says that he will talk to him
38
Suspected Impairment
- Two weeks have passed and nothing appears to have
been done and the pharmacist begins exhibiting
bizarre behavior. - What options do you have?
39
Academic Ethics
- You are taking a pharmacology exam and notice
that one of your fellow students appears to be
referring to note cards in her purse. - The fellow student is also the wife of one of the
pharmacy faculty members. - How would you handle this situation?
40
Institutional Review Board
- You are the member of an Institutional Review
Board reviewing an proposal for a clinical trial
of a new blood pressure medication. - The budget for the trial includes 30 per weekly
visit for unreimbursed expenses for the patient. - Is this coercive?
41
Institutional Review Board
- You review a study for an FDA-approved drug used
for an off-label indication. - The study protocol states that the patient will
be asked to pay for the drug. - What phase clinical trial is this?
- Is it ethical to require the patient to pay for
the drug?
42
Genetic Testing
- Should the public have access to a test to
uncover all genetic predisposion to disease? - Total body CT Scans?
- The market-based system says YES
- if you can afford it, you can buy it!
43
Oregon Health Plan - Rationing
- Rationing not allowed under Federal Medicaid
rules - Oregon received a waiver in early 90s for OHP
- List of diagnoses by medical necessity
- Covered to a specific level based on funding
- Ways to cut costs
- decrease covered patients, diagnoses, payments
- Distributive justice issues?
44
Zevalin
- yttrium-90 (90Y) ibritumomab tiuxetan
- low-grade, follicular, and transformed
non-Hodgkin's lymphoma (NHL) - rare - Approx. 30,000 per monthly treatment
- Longer duration of remission by approximately 3
months - No improvement in survival
45
Erbitux
- Treatment for colon cancer - common
- 17,000 per month
- No evidence of improved survival or quality of
life - Shrinks tumors in 10 of patients
- Covered under most health plans
46
Ethics Case 1
- CC AB is a 47 yof was admitted to the hospital
on 3/6 with recurrent seizures. - HPI This patient was diagnosed with metastatic
cervical carcinoma in January and has been
treated with comfort measures only. She has had
a progressive decline in her ability to care for
herself over the last three weeks.
47
Ethics Case 1
- SH Non-smoker, occasional EtOH, mother
hypertension, father prostate CA, diabetes - FH She is married with two children in their
early twenties. - PE/ROS Neuro patient lethargic and confused.
Unable to communicate.
48
Ethics Case 1
- AB was admitted to the oncology ward, no code
status per husband and POLST. - Over the next several hours her seizures became
more frequent and severe. The family asked the
MD if there is anything you can do to stop the
seizures. - The MD suggested a barbiturate (pentobarbital)
infusion to induce sleep and stop the seizures.
49
Ethics Case 1
- The physician writes an order for pentobarbital
infusion per pharmacy titrate to comfort
50
Ethics Case 1
- What ethical principles are involved
- for the patient?
- for the family?
- for the physician?
- for the pharmacist?
51
Ethics Case 1
- The pentobarbital infusion was started and the
patients seizures stopped and she was deeply
sedated - After four hours of pentobarbital infusion, the
patient stopped breathing and was pronounced dead
52
Ethics Case 1
- What distinguishes this case from assisted
suicide? - Might some people legitimately consider this
assisted suicide? - Could the physician be investigated by the DEA?
53
Ethics Case 2
- You read an article in the morning paper that
half of this years flu vaccine will be lost due
to a manufacturers violation of GMP. - Fortunately, your community pharmacy did not
contract with the manufacturer involved and you
have received 1000 doses of vaccine. - The State Health Division tells vaccine providers
that vaccinating patients who are not in a high
risk category will be fined 500 per vaccination.
54
Ethics Case 2
- The local hospital calls and says that they are
unable to get vaccine because they contracted
with the violating manufacturer and ask (beg!)
for as many doses as you can spare. - What is your answer?
- Any ethics issues involved?
55
Ethics Case 3
- You are working in a busy community pharmacy and
the technician calls you over to counsel on a new
prescription. - The customer is a woman picking up her own
prescriptions and there is also one for her
husband that she had not known about. - The technician set it out for the pharmacist with
the womans prescriptions
56
Ethics Case 3
- The prescription for her husband was an antiviral
drug commonly used for herpes infection. - What should the pharmacist do in this situation?
- What if the prescription was for their sixteen
year-old daughter?
57
Ethics Case 4
- A customer brings a prescription bottle to the
pharmacy counter and tells the clerk that he
would like to speak with the pharmacist. - The pharmacist approaches the counter and the
patient gives her the bottle and says he thinks
that a mistake has been made. - The pharmacist discovers that the bottle was
labeled for ibuprofen 600 mg tablets (30) and
contained warfarin 5 mg tablets.
58
Ethics Case 4
- What steps should the pharmacist take in this
situation?
59
Ethics Case 4
- The customer gives you additional information
that their 13 year-old son has taken six tablets
over the last four days for pain related to a
sprained ankle. - Now what??
60
(No Transcript)