Documentation Training: Part I INSTRUCTIONS - PowerPoint PPT Presentation
1 / 27
Title:
Documentation Training: Part I INSTRUCTIONS
Description:
If prompted to log-in, please enter 'staff' for the user ID and 'scdmh' ... Using SNAPS to develop individualized goals ... or 'None' for any of the SNAPS-please! ... – PowerPoint PPT presentation
Number of Views:55
Avg rating:3.0/5.0
Title: Documentation Training: Part I INSTRUCTIONS
1
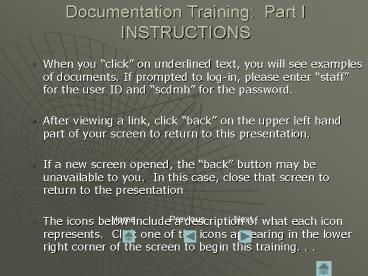
Documentation Training Part IINSTRUCTIONS
- When you click on underlined text, you will see
examples of documents. If prompted to log-in,
please enter staff for the user ID and scdmh
for the password. - After viewing a link, click back on the upper
left hand part of your screen to return to this
presentation. - If a new screen opened, the back button may be
unavailable to you. In this case, close that
screen to return to the presentation - The icons below include a description of what
each icon represents. Click one of the icons
appearing in the lower right corner of the screen
to begin this training. . .
Home
Previous
Next
2
Documentation Training Part One
- How to communicate in writing what you and the
client are doing in treatment
Presented by Charleston-Dorchester MHC-
Quality Improvement Department
Revised 8/06
3
Making the most of this presentation
- There are two parts to this training and all
clinical staff are required to complete both
parts. - It is very important that you write down any
questions as you review these slides, whether
they are general or specific to your area and
contact your Supervisor or us via e-mail
quality improvement or phone 727-2000. - Finally, please feel free to print out the slides
(recommend 3 slides per page with black/white
option) know that you can always come back and
review them at any time.
4
Agenda Part I
- Introduction to Quality Improvement
- 2005 Treatment Service Standards An Overview
- Consents
- Approved Abbreviations
- Plan of Care (POC)
- (aka Individual Treatment Plan ITP)
.
To the left are the items covered in this
presentation. You will need to review both Parts
I and II to receive credit.
5
What is Quality Improvement?
- Quality Improvement is what the Charleston
Dorchester Mental Health Center continuously
strives for - Improving access to our services by people in the
community - Providing best practice services to our
clients - Providing professional development opportunities
for our staff - Increasing the licensure and certification of our
staff - Continuously monitoring the effectiveness and
efficiency of our treatment services and the
satisfaction of our clients
6
Quality Improvement Department
- SUSAN MONOGAN
- M.S ,ED.S.,L.P.C.,N.C.C., L.P.C.S. 727-2000 X
117 - TOM ELLIOTT
- M.S PSYCHOLOGY 727-2000 X 124
- JENNIFER PARKS
- M.Ed., L.P.C., N.C.C.,L.P.C.S. 727-2000 X 115
- JANICE RUDICH
- B.A. PSYCHOLOGY727-2000 X 146
- Initially, the Quality Assurance Dept. was
established to provide a system of monitoring
that assures both internal and external agencies
that the Center is meeting SCDMH Standards
including Corporate Compliance and CARF,
Medicaid/Medicare Standards and HIPAA
Regulations. - Although this is still a large part of our job (
and now include Corporate Compliance) the
Department has evolved over time and its name has
changed to Quality Improvement to reflect the
more proactive aspects of the department and of
their work, e.g. trainings (such as this one
youre doing), consulting with clinical teams to
improve quality of service delivery, and
utilization reviews to determine center-wide
patterns.
7
Our Services and Medicaid
- The services you provide to clients (i.e. STAD,
Individual Therapy, TCM) are based on standards
developed by Medicaid. - An Overview of the Medicaid (DHHS) Treatment
Service Standards may be found on www.cdcmhc.org
, under Staff Only, Quality Improvement, QI
Miscellaneous. - The TX. Service Codes, Descriptions, Units, and
Rates are also available on the CDCMHC web-site. - These are new treatment standards and became
effective February 2005.
8
Medicaid Standards
- The Overview of the 2005 Medicaid Treatment
Services - includes information related to
- Treatment Service Description Codes
- Service Abbreviations
- Whether or not a 2 week staffing is required
- Staffing Ratio
- Lowest Staff Credentials to provide the service
- POC Requirements Whether or not the service
must be listed on the POC and if so what type of
frequency is required - Whether or not a MHP Co-signature is required on
documentation - Treatment Tx Services that Cannot be provided
on the same day
9
Consents
- Be sure to have the legal guardian sign if
patient is under the age of 16. - Persons 16 years of age and older should sign the
consent for treatment and all corresponding
documentation - If other people are participating in treatment,
they need to sign the consent and the
relationship should also be identified on the
consent form. - The signer of the consent should also be the
signer of the POC.
10
Abbreviations
- Part of documentation is saving time through
abbreviations, but you must use abbreviations
that are approved. - An Abbreviation List is located on our website
and in our QI Manual - Should you have recommendations for
abbreviations, please communicate them to the QI
Department.
11
POC Plan of Care(aka ITP Individual
Treatment Plan)
- The Plan of Care (POC) is a working, living
document. As the client progresses in treatment
towards recovery, the goals, objectives,
interventions and services may change. These
changes need to be reflected in the plan of care
12
Using SNAPS to develop individualized goals for a
POC
- Strengths
- What do you enjoy doing? What interests you?
- What kinds of things do you do well?
- What natural talents do you have?
- What aspects of yourself help you keep your
mental and physical health? - Sometimes you may need to provide examples
belief in God, church members are supportive,
love to read, good supportive familyetc. - You may also include clinicians perception of
the clients strengths - Needs
- Are there things you would like to know or learn?
- Are there areas in your life that you need other
people to help you with or do for you?
13
Using SNAPS to develop individualized goals for a
POC
- Needs
- Provide examples if needed money management,
housing, employment - You may also include clinicians perception of
needs - Abilities
- What skills do you have?
- What are you good at doing?
- Provide examples if needed electronic games,
drawing, mechanical - You may also include the clinicians perception
of the clients abilities - Preferences
- Do you have any preferences regarding your
treatment, such as a male or female counselor?
Having your appointments in the morning or early
evening?
14
GOALS
- The goals for the client help to provide a
general direction of treatment. - Goals need to be in the clients own words. If
not possible, these should be stated by a family
member or the therapist - When the client does not state his/her own goals,
this should be indicated on the Plan of Care, in
parentheses under the goal - E.g. (mothers goal) or ( therapists goal)
- Later, when the client is able to actively
participate in goal development the goals should
reflect the clients own words - Examples of goals
- I want to stay out of the hospital
- I dont want to be sad anymore
- I want him to stay in school ( Mothers goal)
- I want to live alone
15
Goals- continued
- Here are some questions you can ask that may help
you with getting appropriate goals - 1. What would you like to get from coming
here? - 2. How do you want me to help you?
- 3. What would you be doing if you werent
having these symptoms/feeling this
way/acting this way? - 4. How would your life be different if you felt
better? - 5. What do you want to change in your life?
16
OBJECTIVES
- Objectives are the behavioral steps that the
client needs to take to achieve their goal(s) - They need to be written so the client knows what
s/he is working on - Objectives must be able to be measured so the
client and you will know when they have been
achieved - Objectives need to be realistic, i.e. based on
what the client thinks they can do, not on what
the clinician thinks the client should do so the
client is able to succeed!
17
Objectives continued
- Examples of Objectives
- 1. Alisha will receive two or less referrals to
the principals office per week as reported by
her teacher ( note the baseline 5 referrals a
week) - 2. Antonio will report two or less panic attacks
per week (note his baseline 4 or more per week)
as reported by client and/or his mother. - 3. Sara will decrease outbursts from 4 times
daily to 1-2 times daily as reported by client
and teacher. - 4. Michael will learn to create a monthly budget
and spend within budget 4/6 months as reported
by client and guardian. - 5. Ahmed will learn to fill his pill minder and
take the meds as prescribed as evidenced by spot
checks of pill minder by counselor and lab
results.
18
INTERVENTIONS
- Interventions are the methods or specific
treatment approaches to be used by the clinician
to help the client meet their objectives - Sometimes the treatment service is the
intervention, e.g. - Clinician will help Jerome work through his
fathers death via individual counseling, 2x
weekly for 60 days. - Other times, you need to cite specific
interventions that will help client accomplish
objective, e.g. - - Clinician will teach La Tasha relaxation
techniques to assist her with trauma issues. - Clinician will use DBT techniques to help client
change her self-destructive behaviors - Clinician will employ role playing to help
change Samuels aggressive behaviors.. - Remember that the interventions cannot
be experimental therapies. They must be
recognized by appropriate profession(s)
19
POC Page 1
- Completed annually.
- Remember you need all 3 signatures on this page.
You and the client must sign the POC. If the
client refuses to sign please indicate so on the
POC. Paybacks occur if the MD does not sign and
date. - Number your goals, (i.e. 1,2,3 etc.) as well as
your objectives /interventions (i.e. 1A, 1B, 2A
) - In the space Type of staff list the lowest
credentialed staff to provide the service. This
can be found on the Overview of the 2005 Medicaid
Treatment Services
20
POC Page 1- continued
- The initial POC must be signed by the MD within
90 days of admission and is effective for 1 year
from the date of admission . - The POC can be written up to 30 days prior to the
renewal (expiration) date with the MD documenting
effective for and then stating the actual
renewal date - e.g. John Smith MD 1-1-06
- (effective for
1-12-06)
21
POC Page 1- continued
- All renewal dates should correspond with the Date
of Admission - If for some reason the renewal date does not
correspond with the Date of Admission - 1. the POC is valid for one year from the MDs
signature - 2. We should ensure that the POC is renewed the
following year on the anniversary of the date of
admission - E.g. according to the MD signature the POC
expires 11/01/06 and the Date of admission is
10-01-06.Renew the POC on 10-01-06 so that from
then on it renews on the Date of Admission
22
POC Page 2
- Please ensure all spaces on the POC are complete,
indicating None at this time or N/A where
appropriate. Do not use NA or None for any of
the SNAPS-please! - Goals for discharge are required to be on all
POCs. - All clinicians providing services to the client
need to be familiar with the POC to write proper
documentation. - Certain services require a Medical Necessity
Statement in addition to being put on the POC
e.g. each type of WRAPS service
23
POC Addendum
- Whenever you initiate this page you must obtain
all three signatures located on the bottom
(client, MHP,MD) - This page expires at the same time as the POC
- At the time of the POC renewal this page also
requires all three signatures (client,MHP,MD)
- Any time you add a service or change a frequency
the MD must initial and date these
additions/changes.
24
POC Addendum
- In order to justify continued treatment, most
clients and their counselors might need to change
goals or objectives, services, and/or frequencies
until all treatment needs are met - This addendum page permits you to add more goals,
objectives and/or services - Addendum pages may be added as needed. Remember
to keep the goal numbers sequential .(e.g.
1.,2.,3.,)
25
POC Progress Summary (90 day 180 day)
- The Progress Summary is required every 90 days
and should coincide with the Date of Admission. - It is important to rate the measurable objectives
of your goals appropriately. If the client has
mastered an objective/goal, it should not be
included on the next POC.
26
POC Progress Summary(270 day 360 day)
- NEW POC TRAINING(8/06) NOW AVAILABLE ON WEBSITE
UNDER QUALITY IMPROVEMENT/TRAINING
- The 360 day Progress Summary also includes a
Annual CARF requirement that you review with the
client their Rights and Responsibilities and
document that in the Progress Summary. It is also
the time to update the Initial Clinical
Assessment. - Adults must document a GAF score at each Progress
Summary - The most recent version of the ITP ( now called
POC) is effective 07/06. - The newest ICA just came out 7/31/06.
27
Conclusion
- Click here to confirm completion of this training
Email Sherri Dangerfield a blank e-mail will
be generated for you to complete. Be sure the
email contains your full name, staff ID, and
office. - Contact the QI Department any questions about
this presentation. - Email Quality Improvement within DMH and
using Groupwise - Email qiu3b_at_scdmh.org outside of DMH
Click here to end