Case - PowerPoint PPT Presentation
1 / 42
Title:
Case
Description:
... medical centers and one community practice, and medical literature ... attributed to ribavirin and thus not investigated further with chest radiography. ... – PowerPoint PPT presentation
Number of Views:33
Avg rating:3.0/5.0
Title: Case
1
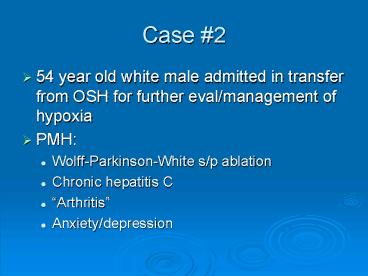
Case 2
- 54 year old white male admitted in transfer from
OSH for further eval/management of hypoxia - PMH
- Wolff-Parkinson-White s/p ablation
- Chronic hepatitis C
- Arthritis
- Anxiety/depression
2
Case 2
- Chronic HCV diagnosed 6/2002 secondary to slight
? LFTs - Referred to NCBH ID for further management 8/2002
- HCV genotype 1a
- HCV VL 2 x 106
- Biopsy 9/9/02 mild periportal chronic
inflammation and piecemeal necrosis early
fibrosis - Self-started PEG IFN/RIB 10/4/2002
3
Case 2 Presentation
- Reports development of progressive SOB symptoms
about the time of initiation of HCV therapy - Symptoms of DOE and non-productive cough
persisted - Evaluated by PCP 10/28/02 and placed on
azithromycin and steroid taper - Symptoms improved transiently and returned
4
Case 2 Presentation
- On re-evaluation by PCP 11/4/02
- Worsened respiratory distress
- CXR revealed diffuse interstitial infiltrates
?pulmonary edema - O2 SAT RA 86
- Admitted to Valdese General for further
evaluation and management
5
Case 2 Presentation
- Extensive work-up included
- r/o MI with serial cardiac enzymes, EKG
- TTE 11/5/02 nl LV fxn PASP 50mmHg
- CT-angiogram chest 11/5/02 alveolar edema and
prominent paratracheal and subcarinal LAD no
evidence of PE - LE dopplers 11/5/02 (-) DVT
- Dobutamine sestamibi 11/6/02 (-) inducible
ischemia - PFTs mild obstruction
6
Case 2 Presentation
- Received aggressive diuresis with some
improvement in SOB - On the evening of 11/8/02, became acutely more
hypoxic - ABG 7.42/30/38/19 78 on ??
- CXR worsening diffuse infiltrates
- Transferred to Valdese MICU and arrangements made
for transfer to NCBH
7
Case 2 Presentation
- On transfer 11/9/02, mild respiratory distress
with 02 sats 90 on 40 FS - ID consulted 11/10/02 for possible role of
hepatitis C therapies, IFN and ribavirin, in
development of acute lung injury
8
CXR 11/10/02
9
CT chest with and without contrast 11/11/02
10
(No Transcript)
11
(No Transcript)
12
(No Transcript)
13
Case 2 Hospital Course
- Bronchoscopy deferred
- CT-guided biopsy of ?lung, paratracheal LN
attempted 11/9/02?unrevealing - Underwent bronch/BAL 11/14/02
- ? cell counts
- GS rare WBC, rare GPC, GNR
- Cx nl throat flora
14
Case 2 Hospital Course
- Decision made to pursue open lung biopsy
- Biopsy performed 11/20/02
15
Open Lung Biopsy
- GS 1 GPC CX 1 CNS
- Pathology all specimens show alterations ranging
from minimally-affected, almost-normal thin
septae to areas of dense fibrosis and
honeycombing. Intermediate features include
active fibrosis andchronic interstitial
inflammation. This heterogenous pattern is best
classified as USUAL INTERSTITIAL PNEUMONITIS
16
Usual interstitial pneumonia (UIP)
- The "usual" pathological finding in patients with
suspected idiopathic pulmonary fibrosis (IPF). - Most cases sporadic and occur in patients who
present in the 5th or 6th decade of life
complaining of slowly progressive dyspnea and
nonproductive cough. - Men are affected more commonly than women by a
ratio of nearly 21. - Rare familial cases of IPF have been described.
17
Usual interstitial pneumonia (UIP)
- Usually follows a relentlessly progressive
course, with most patients dying of respiratory
failure within 5 years of diagnosis. - Periodic exacerbations associated with increased
symptoms and an accelerated decline in pulmonary
function are the rule and can be related to
either variation in the tempo of the underlying
lesion or superimposed complications of various
types.
18
Clinical conditions associated with UIP
- Idiopathic pulmonary fibrosis/cryptogenic
fibrosing alveolitis - Collagen vascular disease
- Drug toxicity
- Chronic hypersensitivity pneumonitis
- Asbestosis
- Familial IPF
- Hermansky-Pudlak syndrome
19
(No Transcript)
20
Pulmonary Complications of Hepatitis C
- Hepatitis C virus-associated
- Therapy associated
21
Extrahepatic manifestations of HCV Disease
- Lymphoproliferative disorders
- Mixed cryoglobulinemia
- Lymphoma
- Other extrahepatic diseases
- Autoimmune thyroiditis
- Sjogrens syndrome
- Idiopathic pulmonary fibrosis
- Dermatologic manifestations
22
HCV and IPF
- Pathogenetic link between HCV infection and IPF
has been suggested by - findings of higher frequency of HCV markers in
IPF patients than in normal controls - observation that some patients with HCV-positive
chronic hepatitis treated with IFN-alpha
developed pulmonary fibrosis
23
HCV and IPF
- Additionally, there was an increased count of
lymphocytes and neutrophils in bronchoalveolar
lavage fluid in patients with HCV chronic
infection, suggesting that HCV infection may
trigger alveolitis. - However, there are conflicting epidemiological
data, mainly from the UK, making this association
an object of debate.
24
HCV and IPF
- Mixed cryoglobulinemia may be complicated by
interstitial lung involvement, suggesting the
association between HCV and IPF may, in some
cases, be indirect, and due to surrounding
HCV-related mixed cryoglobulinemia.
25
Pulmonary complications of alpha-interferon and
ribavirin
- Pulmonary complications of interferon are rare.
- Reported pulmonary complications include
interstitial pneumonitis, pulmonary sarcoidosis,
BOOP, pleural effusion, and exacerbation of
bronchial asthma.
26
Pulmonary complications of a-IFN and
ribavirinRibavirin
- Ribavirin is generally well-tolerated
- Pulmonary side effects such as cough and dyspnea
are common side effects and may make detection of
interferon associated lung injury more difficult
27
Ribavirin Selected Treatment Adverse Events in
Untreated and Relapse Patients
28
RIBAVIRIN
- Role of ribavirin in the development of pulmonary
complications unclear - In previous reports of interferon-related
pulmonary toxicity other than sarcoidosis,
interferon was the only agent used - Could not find any published reports of serious
pulmonary toxicity caused by ribavirin alone
29
RIBAVIRIN
- Ribavirin may have independent pulmonary toxicity
given the frequently associated symptoms of cough
and dyspnea - However,
- Ribavirin monotherapy is no longer used, and in
patients on combination therapy it would be
impossible to exclude interferon as a causative
agent - To date, rates of pulmonary toxicity with
combination interferon/ribavirin seem no higher
than with interferon alone
30
a-interferon and pulmonary toxicity
- Asthma
- Sarcoidosis
- Interstitial lung disease
- BOOP
- Pleural effusions
31
Kumar K, Russo M, Brown R et al. Significant
pulmonary toxicity associated with interferon and
ribavirin therapy for hepatitis C. Am Journal of
Gastroenterology. 2002 97(9) p.2432-2440.
- AIM to analyze the clinical presentation and
outcomes of significant pulmonary toxicity
associated with interferon and ribavirin. - METHODS retrospective review of patients
enrolled in four clinical trials at three sites,
two academic medical centers and one community
practice, and medical literature review.
32
Kumar, Brown et al.
- Four cases of significant pulmonary toxicity were
found or 5.7 of the patients enrolled in the
three studies - Three of the four were on more intensive
interferon regimens with either daily dosing or
pegylated interferon
33
Kumar et al.Clinical Profile of the Four
Patients
34
Kumar, Brown et al.
- Two of three patients on standard interferon
received higher than conventional doses of
interferon suggesting possible dose-dependent
toxicity - No relationship found to severity of liver
disease or the presence or absence of virological
response.
35
Kumar, Brown et al.
- Incidence of pulmonary toxicity in high-dose
studies 5.7 relatively high - During that same time period, NO significant
pulmonary toxicity was seen in the other 500
HCV patients treated in the 3 practices. - Thus, the overall incidence was lt1.
36
Kumar, Brown et al.
- Whether the higher incidence in the high-dose
studies reflected increased scrutiny and thus a
detection bias or a truly increased incidence
with higher doses of is not known. - However, increased surveillance for adverse
effects may be prudent in patients on high-dose
interferon regimens or pegylated interferons.
37
Pulmonary Toxicity of Interferon and
RibavirinConclusions
- Limited number of cases in the literature
illustrate possible serious, but usually
reversible, pulmonary toxicity associated with
interferon therapy. - Pulmonary toxicity is likely more common than
previously believed because symptoms such as
dyspnea or cough may be attributed to ribavirin
and thus not investigated further with chest
radiography.
38
Pulmonary Toxicity of Interferon and
RibavirinConclusions
- Although respiratory symptoms are often observed
with ribavirin, consider further investigation
with pulmonary function tests, arterial blood
gas, or chest x-ray, if symptoms are severe or
persistent as they may reflect underlying
pulmonary toxicity.
39
Pulmonary Toxicity of Interferon and
RibavirinConclusions
- Kumar et al. obtained CXR in all patients with
symptoms of cough or dyspnea that lasted greater
than 2 wk and were severe enough to warrant
consideration of discontinuation of therapy
(510 of treated patients in their experience). - Obtained further workup in patients with abnormal
chest x-rays.
40
Pulmonary Toxicity of Interferon and
RibavirinConclusions
- Though the definition of severity is somewhat
subjective, this appears to be an adequate
screening algorithm because all affected patients
had abnormal x-rays , and no pulmonary toxicity
has developed in the patients without
radiographic changes.
41
Pulmonary Toxicity of Interferon and
RibavirinConclusions
- As the precise mechanism of action of ribavirin
in the treatment of hepatitis C is unclear, its
role if any in causing pulmonary toxicity is
unknown.
42
Case 2
- Did receive high-dose corticosteroid therapy
following open lung biopsy with minimal
improvement - Remained significantly hypoxic with 6-10L
continuous O2 requirement - D/C home with hospice support