Oops forgot one' - PowerPoint PPT Presentation
1 / 23
Title: Oops forgot one'
1
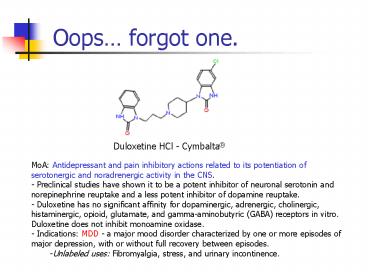
Oops forgot one.
Duloxetine HCl - Cymbalta
- MoA Antidepressant and pain inhibitory actions
related to its potentiation of serotonergic and
noradrenergic activity in the CNS. - - Preclinical studies have shown it to be a
potent inhibitor of neuronal serotonin and
norepinephrine reuptake and a less potent
inhibitor of dopamine reuptake. - Duloxetine has no significant affinity for
dopaminergic, adrenergic, cholinergic,
histaminergic, opioid, glutamate, and
gamma-aminobutyric (GABA) receptors in vitro.
Duloxetine does not inhibit monoamine oxidase. - Indications MDD - a major mood disorder
characterized by one or more episodes of major
depression, with or without full recovery between
episodes. - Unlabeled uses Fibromyalgia, stress, and urinary
incontinence.
2
Hypnotic Agents
- A dose-related, generalized depression (more than
seen with anti-anxiety sedative drugs) of the CNS
that produces drowsiness and induces sleep - Often an increase in the dosage of a sedative
agent will produce hypnotic activity - Ideal hypnotic agent would produce drowsiness and
facilitate the onset and maintenance of sleep
that resembles natural sleep in its
electroencephalographic characteristics and from
which the recipient can be aroused easily - No next-day effects such as rebound anxiety or
continued sedation (Hang Over) - Chronic use without dependence or rebound
insomnia on discontinuation - Insomnia is one of the most common complaints in
general medical practice - Treatment is predicated upon proper diagnosis
- Regular moderate exercise is the best treatment
for insomnia
3
Hypnotic Agents
- Management of insomnia is controversial
- Pharmacological versus non-pharmacological
treatment - Use of short-acting versus long acting hypnotic
agents - Search for specific causes of the problem use
non-pharmacologic treatments when possible. - Are there drug causes for insomnia?
- ethanol use, caffeine containing products or OTC
medications such as decongestants - Sleep hygiene education-no caffeine or
decongestants, no ethanol, adequate exercise,
regular sleep and waking times - Types of insomnia
- Transient less than 3 days and caused by brief
environmental or situational stress - Short-term 3 days to 3 weeks caused by
stressors such as illness, grief or job problems - Long-term insomnia lasting for more than 3
weeks
4
Hypnotic Agents
- Causes of long-term insomnia
- Major psychiatric illnesses and drugs used to
treat - Depression SSRIs in initial stages but will
disappear as the depression is treated - if
insomnia continues trazodone may improve sleep - Anxiety disorders, psychosis such as
schizophrenia - insomnia often disappears as they
begin treatment with dopamine blocking agentsif
agitation continues benzodiazepines are useful
adjuncts - Insomnia due to CHF, asthma, COPD, chronic pain
in terminal cancer (adequate pain control usually
resolves the insomnia) - Conditioned or learned insomnia patients
associate the bedroom with activities other than
sleep - NO TV, reading, or computer use!
- Sleep state misperceptions feel they do not
sleep but it is an illusion - Sleep apnea (hypnotics are CONTRAINDICATED)
sleep studies - Long-term insomnia patients must also adhere to
non-pcol treatments - Sleep restriction therapy, go to bed only when
sleepy, leave the bedroom if sleep does not come
in 15-20 minutes, arise at the same time, avoid
naps
5
Hypnotic Agents
- Side-Effects of hypnotic agents limit their
usefulness - Decreased effectiveness over time
- Rebound insomnia on discontinuation
- All these drugs change sleep architecture
- Barbiturates decrease REM sleep
- Benzodiazepines reduce slow-wave non-REM sleep
- Benzodiazepines produce cognitive changes - next
day confusion, increased rate of falls in the
elderly, rebound next-day anxiety, amnesia,
worsening of sleep apnea - Short-acting agents - rapid sleep but often wake
up after 3-4 hours and can not get back to sleep - Elderly polyphasic sleep pattern (napping) -
siesta - Altered pharmacokinetic activity due to reduced
body water (diuretics), reduced renal function,
increased body fat greatly increased the
half-life for benzodiazepines - Week 1 pleasant sleep and adequate daytime
wakefulness - Week 3 may produce daytime confusion, amnesia,
cognitive impairment and impair quality of life
6
Hypnotic Agents
- Management of patients on long-term treatment
- In elderly termination of benzodiazepines will
be a long, involved process - Seizures, rebound insomnia, altered sleep
patterns - Patients taking these drugs for months or years
are a special problem group - If taking for more than 2 weeks the drug must be
tapered slowly without abrupt discontinuation - In patients on short half-life agents Easier to
switch them to a long half-life agent and taper
dosage - Remember that the withdrawal of long-acting
agents will have DELAYED withdrawal side effects - Use extreme care in discontinuation in patients
with known seizure disorders
7
Hypnotic Agents
- Prescribing Guidelines
- Benzodiazepines, zolpidem, and zaleplon are
preferred over barbiturates greater therapeutic
index - Benzodiazepines with a short half-life are
favored in patients with sleep-onset insomnia and
no daytime anxiety - Benzodiazepines with a longer half-life are
preferred if daytime anxiety is present, tolerate
next-day sedation - Start at small dose and incrementally increase as
necessary - Long half-life agents can accumulate and after
2-4 weeks - Cause next-day cognitive impairment or delayed
daytime cognitive impairment - Benzodiazepines are preferred in the elderly
- Less risk of falls and respiratory depression
- Caution early morning wakening, rebound daytime
anxiety and amnesic episodes - more common at
higher dosage - Avoid barbiturates, glutethimide and meprobamate
(anti-anxiety agent) for insomnia management - High abuse potential and very easy to overdose
8
Barbituate Sedative Hypnotics
- These agents have largely been replaced by the
benzodiazepines due to a higher margin of safety - As hypnotic agents used only for short-term
treatment of insomnia - less than 2 weeks - All are absorbed orally and distributed to all
tissues and body fluids - Lipid solubility as determined by the partition
coeffficient correlates with the pharmacology one
observes - higher the lipid solubility the faster
the onset and the shorter the duration of action - High lipid solubility or hydrophobicity leads to
extensive plasma protein binding - acidic drugs
will result in displacement and increased CNS
depression drug-drug displacement drug
interactions - Tissue redistribution is a result of lipid
solubility differences and the extent of plasma
protein binding - influences rate of excretion
9
Barbituate Sedative Hypnotics
- Sedative (Anxiolytics) and hypnotics are short
and intermediate agents with rapid onset and
short duration - Side-effects
- Decreases the incidence of REM sleep
- Problems are dose-related respiratory
depression, suicide - Idiosyncrasy excitation and hypersensitivity are
possible - Acute overdose coupled with ethanol or other CNS
depressant use is a leading cause of death - Chronic use ? psychological and physical
dependence - Other properties
- Anesthesia ultra-short acting agents quickly
cross BBB then less rapidly redistribute to other
tissues - poor analgesic
- Anti-epileptic and anti-seizure - primarily now
used in a prophylactic treatment to prevent
future seizures
10
Barbituate Sedative Hypnotics
- Metabolism is via CYP450 extent is a function of
the drug itself - Inducers or stimulators of increased production
of these enzymes leading eventually to metabolic
tolerance - Induction leads to increased porphyrin and heme
synthesis and finally the intact CYP450 enzyme - Cross tolerance does develop between the various
agents - Any drug that is metabolized by an induced enzyme
as a result of barbiturate use will be cleared
from the body at a higher than normal rate - Excretion of the free drug and the metabolites
occurs renally as the free acid - Urinary alkalinization will increase the rate of
only phenobarbital due to a favorable pKa value - Alkalinization will not increase excretion of the
other barbiturate due to high pKa values - MOA mimics GABA enhancing inhibitory effects of
GABA by binding the GABA receptor-chloride
channel complex
11
Anticonvulsant Agents
Barbiturates First agent discovered
Indications Grand mal seizures in pediatric
patients, status epilepticus MOA Enhances GABA
mediated chloride influx (GABA inhibition) Metabol
ism Liver metabolism. Stimulates P450 enzymes
that increases the metabolism of MANY
drugs! Given IV or PO with slow onset and a very
long half-life (gt50h) Can cause CNS depression,
drowsiness, and associated in decreased IQ in
chronically treated children.
12
Barbituate Sedative Hypnotics
Short Acting agents Indication short term (lt2
weeks) treatment of insomnia, some use as a
sedative preoperatively as a pre-anesthesia
agent Due to decreased hepatic and renal function
in elderly or debilitated patients decreased
dosage Mild insomnia 100 mg 100 mg Onset
of action 10-15 minutes and a duration of 3-4
hours Half-life 15-50 hours 15-40
hours Pentobarbital is also available in a
suppository dose form and can be used in children
13
Barbituate Hypnotics
Intermediate Acting agents Indication short
term (lt2 weeks) treatment of insomnia, some use
as a sedative (preop) Decrease dosage with
decreased hepatic and renal function in elderly
or debilitated patients Mild insomnia 40-80 mg
(up to 160 mg) 50-100 mg Onset of action
45-60 minutes and a duration of 6-8
hours Half-life 14-34 hours 66-140 hours
14
Non-barbituate Sedative Hypnotics
Indications short-term defined as 1 week
treatment of insomnia 200, 500 and 750 mg
capsules---dose of 500-1000 mg given at bedtime -
give the smallest effective dose to elderly or
debilitated patients Extensive enterohepatic
recirculation of metabolites, use caution in
renal/hepatic impairment MOA sedative hypnotic
with anticonvulsant and muscle relaxant
properties - exact mechanism unknown Indications
3-7 days for insomnia, with a drug free period
of a least 1 week before reuse 250 mg tablets -
dose of 250-500 mg at bedtime - not recommended
for use in children MOA general CNS depressant
with strong anticholinergic activity, suppresses
REM sleep with REM rebound CYP inducing agent,
enterohepatic recirculation
Tertiary Acetylenic Alcohols
Products Piperidines
15
Non-barbituate Sedative Hypnotics
Indications anxiety, emotional stress,
menopausal syndrome, PMS, insomnia, pre- and
postoperative use, spastic colitis MOA
Ring-opened barbiturate, hydrolyzed to urea.
Releases Br- to produce a secondary anion
potentiation of GABA channels in the
CNS Short-acting agent generally replaced by
safer agents - addictive, possible bromide
toxicity (displacement of chloride from the body)
Ureides
Others
Indications nocturnal hypnotic, rectally for
alcohol withdrawl, dental sedation Metabolized to
trichloroethanol, Mickey Finn, MOA??
Indications Sedative/hypnotic, DTs Hepatic
metabolized, excreted renally and by breathing,
nasty smelling breath
16
Non-barbituate Sedative Hypnotics
Indications Management of anxiety,
effectiveness of gt 4 months is unknown hospital
use MOA a carbamate derivative that has
multiple CNS sites of action by inhibiting
neurotransmission in the thalamus and limbic
system, inhibits multi-neuronal spinal reflexes.
Acts like benzodiazepines, but less selective and
higher abuse potential. 200, 400 and 600 mg
tablets May cause seizures in epileptics, notify
MD if pregnant or planning, withdrawl can lead to
seizures
This drug is also found (as you know) with the
antianxiety agents!!!
17
Non-barbituate Sedative Hypnotics
Indications preoperative or during surgery
sedative, adjunct to labor analgesia Short
duration of action injection only agent MOA a
phenothiazine with sedative, anti-emetic and
antihistaminic properties With narcotics,
decrease dosage of narcotic by 25-50 Indications
sedation of ICU patients that are intubated
and mechanically ventilated, presurgical use in
minor gyn surgery, tubal ligations and opthalmic
surgery Injection only MOA relatively
selective a2 receptor agonist Clonidine congener
(Blood-pressure reducing agent) Hepatic
glucuronidation and renal excretion
18
Non-barbituate Sedative Hypnotics
Pyrazolopyrimidines
Indications Short-term management of
insomnia 5, 10 mg capsules 5-20 mg total dosage
but use caution and lower doses in hepatic
failure and elderly low dependency tolerance
risk MOA specific binding of the GABA-BZ omega1
receptor complex Japanese subjects up to 37
concentration increase due to metabolic CYP
differences, amnesia and unusual behavior changes
possible
Zaleplon - Sonata
Imidoazopyridines
Indications Short-term treatment of insomnia 5
and 10 mg tablets with maximum of 10 mg
immediately before bed low dependency
risk Decrease dose in hepatic impairment or in
combo with other CNS depressants due to additive
effect MOA non-benzodiazepine modulation of the
GABA-BZ receptor chloride channel complex No
myorelaxant or anticonvulsant properties
19
Non-barbituate Sedative Hypnotics
Pyrrolopyrazine
Eszopiclone - Lunesta
- Insomnia
- MoA unknown believed to result from
GABA-receptor complexes at binding domains
located close to or allosterically coupled to
benzodiazepine receptors. - Metabolized by CYP3A4 and CYP2E1 via
demethylation and oxidation - Interactions
20
Non-barbituate Sedative Hypnotics
Benzodiazepines
Indications Insomnia MOA potentiates GABA
neuronal inhibition by interacting with the GABA
chloride ion channel receptor complex same as
the anti-anxiety agents! Hypnotic dosages 1-2
mg 15-30 mg 15-30 mg Peak levels 2
hours 0.5-1 hour 1.2-1.6
hours Half-life 8-28 hours 50-98 hours
3.5-18.4 hours All are tightly protein bound
gt90, hepatic metabolism
21
Non-barbituate Sedative Hypnotics
Benzodiazepines continued
Indications Hospital sedation,
insomnia Insomnia MOA potentiates GABA
neuronal inhibition by interacting with the GABA
receptor complex Hypnotic dosages 0.125-0.5
mg 7.5-15 mg Peak levels 1-2 hours 1-2
hours Half-life 1.5-5.5 hours 47-100
hours Tightly protein bound, hepatic
metabolism Similar to flurazepam, much more
Triazolam should not be used by patients
unless a full nights sleep is obtained and
adequate time is given for elimination prior to
activity - amnesia is possible
22
New for 2005
- Rozerem (ramelteon) Tablets
- Approved July 22, 2005 Company Takeda
Pharmaceuticals North America, Inc. - Treatment for InsomniaRozerem is the first and
only prescription sleep medication that has shown
no evidence of abuse and dependence, and is
therefore not designated as a controlled
substance. Rozerem is indicated for the treatment
of adults with insomnia characterized by
difficulty with sleep onset, and can be
prescribed for long-term use.
23
Ramelton - Rozerem
- Indication treatment of adults with insomnia
characterized by difficulty with sleep onset, and
can be prescribed for long-term use. - MoA Melatonin receptor agonist at the MT1 and
MT2 receptors - Metabolized primarily by CYP1A2, also 3A4 and 2C
families to a lesser degree. - Warnings Not used in renal impairment, can cause
cognitive impairment, Not to be taken with
alcohol, appears to decrease tesosterone and
increase prolactin. No data yet for pediatric use