P1254325912lqoHp - PowerPoint PPT Presentation
1 / 24
Title:
P1254325912lqoHp
Description:
Results from excessive host response to prior infectious process which has ... and coalesce into an inflamed caseous mass referred to as mediastinal granuloma ... – PowerPoint PPT presentation
Number of Views:134
Avg rating:3.0/5.0
Title: P1254325912lqoHp
1
(No Transcript)
2
(No Transcript)
3
Fibrosing Mediastinitis
- Morning Report
- Liz Thomas
- July 25, 2008
4
Overview
- Fibrosing mediastinitis is characterized by an
excessive fibrotic reaction in the mediastinum
which can compromise the great vessels, airways,
or other structures in the mediastinum - Results from excessive host response to prior
infectious process which has involved the
mediastinal lymph nodes, usually thought to be
due to Histoplasma capsulatum, although has also
been suggested to result from TB, syphilis,
blastomycosis, autoimmune process, drugs or trauma
5
H. Capsulatum
- Histoplasmosis was first described in 1906 by a
US Army physician in Panama - Infection is common and usually subclinical
- H. capsulatum is found worldwide, but in the US,
infection is most common in the midwestern states
located in the Ohio and Mississippi River valleys - The fungus proliferates in soil contaminated with
bird or bat droppings, commonly chicken coops or
farms buildings, bird roost sites, caves, and
wood lots
6
Distribution of Pulmonary Histoplasmosis
7
Chicken coop
8
Pathophysiology
- H. capsulatum conidia or mycelial fragments are
inhaled and, if they evade nonspecific lung
defenses, cause a localized or patchy
bronchopneumonia - With low-inoculum exposure, most healthy
individuals remain asymptomatic (fewer than 5
develop symptomatic disease) - Patients who inhale a large inoculum often
develop severe and potentially fatal diffuse
pulmonary infection
9
Histoplasma capsulatam
10
Pathophysiology
- Macrophages ingest the fungi and disseminate the
infection hematogenously during the first 2 weeks
of infection - May result in development of H. capsulatum
containing granulomata in the liver and spleen,
usually discovered incidentally or at autopsy - Clinically evident dissemination usually occurs
only in patients with underlying
immunosuppressive disorders, those at extremes of
age, and patients with a heavy exposure
11
Pathophysiology
- Cellular immunity develops after 10-14 days,
first in the lungs and mediastinal lymph nodes
and then throughout the reticuloendothelial
system - Sensitized T lymphocytes activate macrophages and
the infection is brought under control in
immunocompetent hosts - Reinfection with H. capsulatum may bring about a
heightened immune response, resulting in intense
inflammation of the pulmonary parenchyma - This response may play a role in the caseating
tissue necrosis seen in some patients, including
those with chronic pulmonary manifestations such
as fibrosing mediastinitis and a sarcoidosis-like
syndrome
12
Mediastinal granuloma
- Mediastinal lymph nodes invaded by H. capsulatum
may enlarge and coalesce into an inflamed caseous
mass referred to as mediastinal granuloma - Usually presents as a mediastinal mass discovered
incidentally or because it compresses compliant
mediastinal structures such as the SVC or
esophagus. - The lymph nodes are generally easily removed
surgically, and the process is more common and
more benign than fibrosing mediastinitis
13
Fibrosing Mediastinitis
- Believed to result from leakage of fungal
antigens from lymph nodes into the mediastinal
space, leading to a hypersensitivity reaction and
fibrotic response - Fibroblasts adjacent to granulomata are
stimulated and proliferate, leading to fibrosis,
entrapment, and invasion of adjacent normal
structures - Unclear whether mediastinal granuloma can
progress to mediastinal fibrosis or if the two
entities are distinct
14
Epidemiology
- Although it is estimated that over 500,000 people
per year in the US are infected with Histoplasma
and over 80 of inhabitants of endemic regions
have a positive Histoplasma skin test, less than
1 of patients with histoplasmosis develop
fibrosing mediastinitis - The largest case series (which describes only 94
patients) showed that the average age of
diagnosis was 33, 81 were white, and there was a
slight male preponderance
15
Clinical presentation
- Depends upon the structures involved (airways,
heart and great vessels, or the esophagus) - Compression of the tracheobronchial tree can lead
to dyspnea, postobstructive pneumonia,
atelectasis or broncholithiasis due to bronchial
erosion by calcified lymph nodes - Involvement of heart and great vessels can lead
to pulmonary artery or vein obstruction, SVC
syndrome, and constrictive pericarditis - Esophageal compression can lead to dysphagia or
odynophagia
16
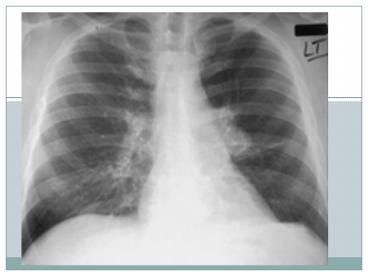
Imaging studies
- CXR May see hilar or mediastinal adenopathy,
lobar or segmental consolidation, unilateral
small pulmonary artery, septal lines, pleural
effusion, or cardiomegaly - CT Can show infiltrative mediastinal process
with or without discrete mass, often shows
calcifications within the mediastinal process - MRI Typically reveals a heterogeneous mass
decreased signal intensity on T2 weighted images
suggests fibrosis
17
CT of a 30 year old man with SVC syndrome
secondary to fibrosing mediastinitis
- Contrast-enhanced CT scan (mediastinal window)
shows an infiltrating soft-tissue attenuation
mass in the middle mediastinum. Note encasement
and narrowing of the distal superior vena cava
(white arrowhead) and right pulmonary artery
(black arrowheads) and distention of the azygous
vein (arrow).
18
Biopsy
- The differential diagnosis for noncalcified
mediastinal mass includes lymphoma and carcinoma,
so patients with fibrosing mediastinitis usually
undergo biopsy to confirm the diagnosis - Biopsy is done first and foremost to exclude
malignancy - Histology generally shows abundant collagen
containing cellular fascicles of fibroblasts
associated with a chronic inflammatory
infiltrate. Aggregates of lymphocytes and plasma
cells are found within a hyalinised fibrous
connective tissue
19
Histology
- Fibrous tissue infiltrating mediastinal adipose
tissue
- Paucicellular, eosinophilic mature collagen
20
Treatment
- There are no known effective medical therapies
for fibrosing mediastinitis - Some case reports have found symptomatic
improvement with steroids and it has been
suggested that autoimmune processes respond more
favorably - Case reports have also shown improvement of
symptoms with Tamoxifen - Antifungal agents are generally ineffective
- Surgery is sometimes performed to relieve
vascular and airway obstruction, with variable
success
21
Surgical treatment
- SVC obstruction SVC bypass has been performed
successfully in some patients, both with spiral
vein grafts and with endovascular stents - Airway compression Relief of airway obstruction
generally requires resection of the airway and/or
lung parenchyma, as dilation of the airways is
usually not feasible. This type of surgery is
associated with significant mortality - Esophageal involvement Esophageal compression
and tracheoesophageal fistula may be managed with
stents and/or surgical correction
22
SVC stent
23
Prognosis
- Fibrosing mediastinits is a progressive disease
with no definitive treatment and with a variable
natural history - One series of 23 patients found that 10 had
improvement in symptoms, 11 had no significant
change, and two had progressive disease - Another series of 71 patients noted a worse
prognosis, with 21 patients dying during
follow-up. The mean interval between development
of symptoms and death was less than 6 years in
these patients.
24
References
- Manali ED, Saad CP, Krizmanich G, Mehta AC.
Endobronchial findings of fibrosing
mediastinitis. Respir Care. 2003
Nov48(11)1038-42. - Flieder DB, Suster S, Moran CA. Idiopathic
fibroinflammatory (fibrosing/sclerosing) lesions
of the mediastinum a study of 30 cases with
emphasis on morphologic heterogeneity. Mod
Pathol. 1999 Mar12(3)257-64. - Bays S, Rajakaruna C, Sheffield E, Morgan A.
Fibrosing mediastinitis as a cause of superior
vena cava syndrome. Eur J Cardiothorac Surg.
2004 Aug26(2)453-5. - Pompeo E, Stella F, Ippoliti A, Mineo TC.
Extra-anatomic bypass of the superior vena cava
after successful stenting for fibrosing
mediastinitis. J Thorac Cardiovasc Surg. 2008
Jan135(1)220-1, 221.e1 - Ikeda K, Nomori H, Mori T, Kobayashi H, Iwatani
K, Yoshimoto K, Yoshioka M. Successful steroid
treatment for fibrosing mediastinitis and
sclerosing cervicitis. Ann Thorac Surg. 2007
Mar83(3)1199-201. - UpToDate 2008