ESH/ESC Guidelines: PowerPoint PPT Presentation
1 / 77
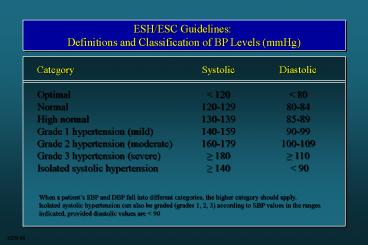
Title: ESH/ESC Guidelines:
1
ESH/ESC Guidelines Definitions and
Classification of BP Levels (mmHg)
Category Optimal Normal High normal Grade 1
hypertension (mild) Grade 2 hypertension
(moderate) Grade 3 hypertension (severe) Isolated
systolic hypertension
Systolic lt 120 120-129 130-139 140-159 160-179
180 140
Diastolic lt 80 80-84 85-89 90-99 100-109 110
lt 90
When a patients SBP and DBP fall into different
categories, the higher category should
apply. Isolated systolic hypertension can also be
graded (grades 1, 2, 3) according to SBP values
in the ranges indicated, provided diastolic
values are lt 90
6254 M
2
CHD and usual BP (in 5 categories defined by
baseline DBP) 9 prospective observational
studies 4856 events
Stroke and usual BP (in 5 categories defined by
baseline DBP) 7 prospective observational
studies 843 events
Relative Risk of Stroke
Relative Risk of Stroke
Baseline DBP category Usual SBP Usual DBP
Baseline DBP category Usual SBP Usual DBP
1
2
3
4
5
1
2
3
4
5
123 76
136 84
148 91
162 99
175 105
123 76
136 84
148 91
162 99
175 105
Approximate mean usual BP (estimated from later
remeasurements in the Framingham Study)
Approximate mean usual BP (estimated from later
remeasurements in the Framingham Study)
Collins R and McMahon S, British Medical Bulletin
1994
3510
3
- JNC 7
- Individuals with
- SBP of 120-139 or DBP of 80-89 mmHg should be
considered as prehypertensive - and require health promoting
- lifestyle modifications to prevent CVD
4
4-Year Frequency () of Progression to HT
according to BP Values within Normal Range (n
9845, Framingham)
35-64 ys
65-94 ys
49.5
37.3
25.5
17.6
16.0
5.3
Data adjusted for sex, age, BMI, baseline
examinations
Vasan et al., Lancet 2001 358 1682
7395 M
5
Prehypertension - Criticism
Progression to HT less frequent in several
studies Hypertension has an ominous
significance by the layman Anxiety over the term
may create need for medical visits / lab
examinations Several lifestyle changes must be
preceded by / performed under medical check /
guidance Lifestyle changes - Not invariably
devoid of cost - Reflection on subjects QoL,
freedom etc.
8222 M
6
ESH/ESC Guidelines Stratification of Risk to
Quantify Prognosis
Blood Pressure (mmHg)
Grade 1 SBP 140-159 or DBP 90-99
Grade 2 SBP 160-179 or DBP 100-109
Grade 3 SBP 180 or DBP 110
Normal SBP 120-129 or DBP 80-84
High Normal SBP 130-139 or DBP 85-89
Other Risk Factors and Disease History No other
risk factors 1-2 risk factors Associated
Clinical Conditions
High added risk
Moderate added risk
Low added risk
Average risk
Average risk
Very high added risk
Moderate added risk
Moderate added risk
Low added risk
Low added risk
Very high added risk
High added risk
High added risk
High added risk
Moderate added risk
3 or more risk factors or TOD or diabetes
Very high added risk
Very high added risk
Very high added risk
Very high added risk
High added risk
Low risk lt 15 Medium risk 15-20 High risk
20-30 Very high risk gt 30
7772 M
7
ESH/ESC Guidelines Factors Influencing Prognosis
Risk factors for CV disease used for
stratification Levels of SBP and DBP Men gt 55
years Women gt 65 years Smoking Dyslipidaemia (t
otal chol. gt 250 mg/dl, or LDL-chol. gt 155 mg/dl,
or HDL-chol. M lt 40, W lt 48 mg/dl Family history
of premature CV disease (at age lt 55 years M, lt
65 years W) Abdominal obesity (abdominal
circumference gt 102 cm, W gt 88 cm) C-reactive
protein gt 1 mg/dl
Target Organ Damage (TOD) Left ventricular
hypertrophy (electrocardiogram Sokolow-Lyons gt
38 mm Cornell gt 2440 mmms echocardiogram LVM
I gt 125, W gt 110 g/m2) Ultrasound evidence of
arterial wall thickening (carotid IMT gt 0.9 mm)
or atherosclerotic plaque Slight increase in
serum creatinine (M 115-133, W 107-124 ?mol/l M
1.3-1.5, W 1.2-1.4 mg/dl) Microalbuminuria (30-30
0 mg/24h albumin-creatinine ratio M gt 22, W gt 31
mg/g M gt 2.5, W gt 3.5 mg/mmol)
Diabetes Mellitus Fasting plasma glucose 7.0
mmol/l (126 mg/dl) Postprandial plasma glucose gt
1.0 mmol/l (198 mg/dl)
Associated Clinical Conditions (ACC) Cerebrovascu
lar disease ischaemic stroke cerebral
haemorrhage transient ischaemic attack Heart
disease myocardial infarction angina coronary
revascularization congestive heart
failure Renal disease diabetic
nephropathy renal impairment (serum creatinine M
gt 1.5, W gt 1.4 mg/dl) proteinuria (gt 300
mg/24h) Peripheral vascular disease Advanced
retinopathy haemorrhages or exudates,
papilloedema
6250 M
8
HT
BP (mmHg)
RRR ()
NT
BP (mmHg)
RRR ()
PROGRESS, Lancet 2001
8236 M
9
Stroke More vs less CHD More vs
less Heart failure More vs less Major CV
events More vs less CV death More vs
less Total mortality More vs less
Mean BP ? (mmHg) -4 / -3 -4 / -3 -4 / -3 -4
/ -3 -4 / -3 -4 / -3
Relative Risk (95 CI) 0.77 (0.63-0.95) 0.86
(0.72-1.03) 0.84 (0.59-1.18) 0.86
(0.77-0.96) 0.93 (0.77-1.11) 0.96 (0.84-1.09)
Favours active
Favours control
0.5
1.0
2.0
Relative risk
8175 6397 alt. M
10
RR of CVD with Low-Dose Aspirin (vs Placebo) in
HOT
On-treatment BP (mmHg) Medium risk High / very
high risk
140/83 1.00 0.78
statistically significant
Zanchetti et al., J Hypertens 2002 20 2309
8247 M
11
On-Treatment BP and ? Events with Atorvastatin
(vs Placebo) in ASCOT
All patients with 3 risk factors BP
(mmHg) 138/80 Stroke -27 CHD -2
9 CVD -21 Total mortality -13 (NS)
8248 M
12
Initiation of Antihypertensive Treatment
Blood Pressure (mmHg)
Grade 1 SBP 140-159 or DBP 90-99
Grade 2 SBP 160-179 or DBP 100-109
Grade 3 SBP 180 or DBP 110
Normal SBP 120-129 or DBP 80-84
High Normal SBP 130-139 or DBP 85-89
Other Risk Factors and Disease History No
other risk factors 1-2 risk factors 3 or
more risk factors or TOD or diabetes Associated
clinical conditions
Immediate drug treatment and lifestyle changes
Lifestyle changes for several months Then drug
treatment
Lifestyle changes for several months Then drug
treatment if preferred by the patient and
resources available
No BP intervention
No BP intervention
Immediate drug treatment and lifestyle changes
Lifestyle changes for several months Then drug
treatment
Lifestyle changes for several months Then drug
treatment
Lifestyle changes
Lifestyle changes
Immediate drug treatment and lifestyle changes
Drug treatment and lifestyle changes
Drug treatment and lifestyle changes
Drug treatment and lifestyle changes
Lifestyle changes
Immediate drug treatment and lifestyle changes
Immediate drug treatment and lifestyle changes
Immediate drug treatment and lifestyle changes
Immediate drug treatment and lifestyle changes
Drug treatment and lifestyle changes
13
Association of Hypertension with Other CAD Risk
Factors Framingham Study
One 26
One 27
Two 25
Two 24
None 19
None 17
Three 22
Three 20
Four or more 8
Four or more 12
Men
Women
Kannel, Am J Hypertens 2000 13 3S-10S
2313
14
Echocardiography and US TSA in Low Risk
HypertensivesAPROS STUDY RISK RE-CLASSIFICATION
Cuspidi et al, J Hypertens 2002
15
Risk Factors in Subjects of the SMOOTH Study with
BP from Optimal to Untreated HT
7637 M
16
JNC VII Classification and Management of Blood
Pressure for Adults Agfed 18 years and Older
Initial drug therapy
Lifestyle modification
DBP mmHg
SBP mmHg
BP classification
With compelling indications
Without compelling indication
Encourage
and lt80
lt120
Normal
Drug(s) for compelling indications.
No antihypertensive drug indicated.
Yes
or 8089
120139
Prehypertension
Drug(s) for the compelling indications. Other
antihypertensive drugs (diuretics, ACEI, ARB, BB,
CCB) as needed.
Thiazide-type diuretics for most. May consider
ACEI, ARB, BB, CCB, or combination.
Yes
or 9099
140159
Stage 1 Hypertension
Two-drug combination for most (usually
thiazide-type diuretic and ACEI or ARB or BB or
CCB).
Yes
or gt100
gt160
Stage 2 Hypertension
Treatment determined by highest BP
category. Initial combined therapy should be
used cautiously in those at risk for orthostatic
hypotension. Treat patients with chronic kidney
disease or diabetes to BP goal of lt130/80 mmHg.
6273 M
17
Clinical Outcomes (6 yr rate .100 persons) in
ALLHAT
CHD Stroke CHF ESRF
A 11.3 5.4 10.2 2.1
L 11.4 6.3 8.7 2.0
C 11.5 5.6 7.7 1.8
P lt 0.02
P lt 0.01
4673 M
18
(No Transcript)
19
Trials on New vs Old TreatmentsPrimary
Endpoints (RR 95 CI)
CAPPP STOP2 ANBP2 ALLHAT STOP2 NORDIL INSIGH
T ALLHAT INVEST ALLHAT SCOPE LIFE
ACE-I ACE-I ACE-I ACE-I CCB CCB CCB CCB CCB ?B ARB
ARB
n 10985 n 4418 n 6083 n 9054 n
4209 n 10881 n 6321 n 9048 n 22599 n
24335 n 4506 n 9193
1.05 (0.90-1.22) 1.01 (0.84-1.22) 0.89
(0.79-1.00) 0.99 (0.91-1.08) 0.97
(0.80-1.17) 1.00 (0.87-1.15) 1.10
(0.91-1.34) 0.98 (0.90-1.07) 0.98
(0.90-1.06) 1.03 (0.90-1.17) 0.89
(0.75-1.06) 0.87 (0.77-0.98)
0.5
1.0
2.0
CVD CHD
New better
Old better
Mancia G. et al., 2003
5487 M
20
ANBP2 Primary End-Points among All, Male, and
Female Subjects
All Subjects End Point All CV events or death
from any cause First CV event or death from any
cause Death from any cause Male Subjects End
Point All CV events or death from any cause First
CV event or death from any cause Death from any
cause Female Subjects End Point All CV events
or death from any cause First CV event or death
from any cause Death from any cause
Hazard Ratio (95 CI) 0.89 (0.79-1.00) 0.89
(0.79-1.01) 0.90 (0.75-1.09) Hazard Ratio (95
CI) 0.83 (0.71-0.97) 0.83 (0.71-0.97) 0.83
(0.66-1.06) Hazard Ratio (95 CI) 1.00
(0.83-1.21) 1.00 (0.83-1.20) 1.01 (0.76-1.35)
P Value 0.05 0.06 0.27 P Value 0.02 0.02 0.14
P Value 0.98 0.98 0.94
ACE-I superior
Diuretics superior
0.2
1.0
5.0
ACE-I superior
Diuretics superior
0.2
1.0
5.0
ACE-I superior
Diuretics superior
0.2
1.0
5.0
Wing et al., N Engl J Med 2003 348 583-92
5370 M
21
All Cardiovascular Events
Number of events / patients
Trials MIDAS/NICS/VHAS STOP2/CCBs NORDIL INSIGHT
ALLHAT/Aml ELSA CCBs without CONVINCE Het. p
0.78 CONVINCE All CCBs Het. p
0.86 UKPDS STOP/ACEIs CAPPP ALLHAT/Lis ANBP2 All
ACEIs Het. p 0.006 LIFE SCOPE All ARBs Het.
p 0.69 ALLHAT/Dox All Trials Het. p lt 0.0001
Old 37/ 1358 637/ 2213 453/ 5471
397/ 3164 3941/15255 33/ 1157 5498/28618
365/ 8297 5863/36915 78/ 358 637/
2213 401/ 5493 3941/15255 429/
3039 5486/26358 588/ 4588 268/ 2460 856/
7048 2245/15268 7627/53279
New 39/ 1353 636/ 2196 466/ 5410
383/ 3157 2432/ 9048 27/ 1177 3983/22341
364/ 8179 4347/30520 107/ 400 586/
2205 438/ 5492 2514/ 9054 394/
3044 4039/20195 508/ 4605 242/ 2477 750/
7082 1592/ 9067 10728/67295
Difference (SD) 3.6 (2.4) 2p
0.14 3.4 (2.3) 2p 0.15 2.6 (3.6) 2p
0.59 -14.3 (5.5) 2p 0.004 1.4 (4.8) 2p
0.69
Odds ratios (95 CIs)
.
.
0
1
2
3
New drugs better
Old drugs better
Staessen, J Hypertens 2003
5563 M
22
CVD and HTN
Antihypertensive T reduces CVD Benefit with a
variety of drug classes D BB ACEI CA ARB BP
reduction per se major factor
4662 M
23
Relative risk of outcome event
SBP difference between randomized groups (mmHg)
7939 6398 M mod.
24
Risk of CVD according to SBP Control by Treatment
CHF
Prior MI
Diabetes
Prior Stroke / TIA
Renal Impairment
Age
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
70
gt 70
30.2
29.8
?
24.6
24.1
?
21.0
20.3
18.9
18.7
17.4
?
?
14.8
14.0
13.6
13.5
12.4
12.4
11.9
11.9
10.8
7.9
7.4
7.4
6.7
6.4
5.1
140 mmHg
P lt 0.001 ? P 0.03 P 0.04
lt 140 mmHg
Pepine, Koney, Kupfer, Benetos, Mancia et al.,
2004
8273 M
25
Hypertension in High-Risk Patients Number of
Agents Required to Achieve BP Goal
UKPDSUnited Kingdom Prospective Diabetes Study
MDRDModification of Diet in Renal Disease
HOTHypertension Optimal Treatment AASKAfrican
American Study of Kidney Disease
RENAALReduction of Endpoints in NIDDM with the
Angiotensin II Antagonist Losartan
IDNTIrbesartan Diabetic Nephropathy Trial
MAPmean arterial pressure.
Bakris et al. Am J Kidney Dis. 200036646-661
Brenner et al. N Engl J Med. 2001345861-869 Lew
is et al. N Engl J Med. 2001345851-860
5129 M
26
2003 ESH/ESC Guidelines
Diuretics
AT1-receptor blockers
ß-blockers
Calcium antagonists
?1-blockers
ACE inhibitors
6220 M
27
2003 ESH/ESC Guidelines
Consider Untreated BP level Absence or presence
of TOD and risk factors Choose between If
goal BP not achieved If goal BP not achieved
Single agent at low dose
Two-drug combination at low dose Two-thre
e drug combination at effective doses
Previous agent at full dose
Switch to different agent at low dose
Previous combination at full dose
Add a third drug at low dose
Two-three drug combination
Full dose monotherapy
6219 M
28
ESH/ESC Guidelines
Particular attention should be given to adverse
events, even primarily subjective disturbances,
because they may be an important cause of
non-compliance Pts should always be asked about
adverse effects and doses or drugs changed
accordingly
6375 M
29
ESH/ESC Guidelines - Specific Indications for
Drug Classes
Thiazides Loop diuretics Antialdosterone
D ?B CCB (DHP) CCB (non-DHP) ACEI ARB ?B
CHF / Elderly / ISH / Blacks Renal insufficiency
/ CHF CHF / Post-MI Angina / Post-MI / CHF /
Pregnancy / Tachyarrhythmias Elderly / ISH /
Angina / PVD / Ca atherosclerosis /
Pregnancy Angina / Ca atherosclerosis / Suprav.
tachycardia CHF / LV dysfunction / Post-MI /
Non-DN / Type I DN / Proteinuria Type 2 DN /
Diabetic microalbuminuria / Proteinuria / LVH /
ACEI-cough BPH / Hyperlipidaemia
6372 M
30
1993 ESH/ESC Guidelines Antihypertensive
Treatment in DM
Non-pharmacological measures (particularly weight
loss and ? Na intake) in all patients BP goal a
130/80 mmHg Combination T required most
often Use of all effective / well tolerated
agents recommended Renoprotection benefits from
regular inclusion in combination T of - ACEI in
type I DM - ARB in type II DM In type II DM
with normal BP use first a RAS blocker Microalbum
inuria (type I/II DM) is an indication for T,
especially with RAS blocker, irrespective of BP
values
6262 M
31
Risk Factors
Subclinical Organ Damage
Events
Not surrogate but intermediate end-point
7997 M
32
LVH Regression by Different Classes of
Antihypertensive Drugs
Calcium antagonists
Ag II- Blockers
Diuretics
?-Blockers
ACE-I
Reduction of LVM ()
p lt 0.01
p lt 0.01
p lt 0.05
Klingbeil A, Schmieder RE, Curr Cardiol Report
2003
6362 M
33
HOPEReduction in Primary Outcome with
Regression/Prevention of LVH
0.20
Proportion of all patients with primary
outcome (CV death, MI, stroke)
P 0.0061
0.15
Development / Persistence
0.10
0.05
Regression / Prevention
0.00
2000
1500
1000
500
0
Days of follow-up
whether or not hospitalized
Mathew J et al., Circulation 2001 104 1615-1621
5811 M
34
New DM in Antihypertensive Drugs Trials
CAPPP ACEI vs Conv
STOP-2 ACEI vs Conv
ALLHAT ACEI vs D
HOPE ACEI vs PL
STOP-2 CA vs Conv
STOP-2 ACEI vs CA
LIFE ARB vs BB
SCOPE ARB vs Conv
CHARM ARB vs PL
INVEST CA vs Conv
INSIGHT CA vs D
ALLHAT CA vs D
-2
-2
-4
-16
-14
-16
-20
-21
-23
-25
-30
-25
-34
-40
T, 2 yrs T, 4 yrs
8092 M 4850 new
35
Rate of Metabolic Syndrome and New Onset Diabetes
in ALPINE after 1 Year T
Candesartan HCTZ
B 13 (6.6) 12 (6.1)
T 5 (2.6) 18 (9.2)
Diabetes 1 (0.5) 8 (4.1)
Metabolic Syndrome
Lindholm et al., J Hypertens 2003 21 1563
8270 M
36
Importance (Hazard Ratio) of ? Blood Glucose at
Age 50 to 60 on Risk of MI after 60
Antihypertensive T (mainly D/BB)
Yes (n 291) 1.37 1.04 0.88 0.11 0.96 0.99 0.
85 0.92
No (n 1358) 1.14 1.16 0.98 1.19 1.25
1.27 1.01 1.26
? Glucose Glucose ? BMI BMI ? SBP SBP ? DBP DBP
P 0.0004 P 0.02 P 0.01
Dunder et al., BMJ 2003, 326
6232 M
37
1625
38
JNC 7 - Stage I Hypertension
As it is Improved Further improvement Ideal
Thiazide diuretics for most May consider ACEI /
ARB / CCB or combination Thiazide diuretics For
most may consider ACEI / ARB / CCB or
combination Thiazide diuretics For most may
consider ACEI / ARB / CCB / BB or, more
frequently, combination T ESH/ESC Guidelines
6701 M
39
Percent of Italian Hypertensives with BP Control
(lt140/90 mmHg) after Year 2000
Forlife ? (n 12792)
SMOOTH (n 2144 )
Mancia et al. ? J Hypertension 2004, 2 (n 3812)
12.2
21.7
14.0
Practitioners
Practitioners
Specialists
? Hypertensives enrolled by physicians across
Italian territory Population survey in San
Marino - n refers to hypertensive fraction
8234 M
40
Effects of antihypertensive agents on changes in
proteinuria and albuminuria in patients with
type 1 and 2 diabetes mellitus (meta-regression
analysis, 100 studies, 2494 patients)
Proteinuria
0.2
Albuminuria
-0.0
Log change from baseline
-0.2
-0.4
ACE Inhibitors
Calcium Channel Blockers
b-blockers
Control
-0.6
Kasiske et al Ann Intern Med 1993
5993 M
41
CBMmax Final Scan versus Baseline Scan
0.06
Atenolol
Mean Change
(mm)
Lacidipine
0.05
0.04
0.03
0.02
0.01
0
ITT
PP 1
PP 2
Compl.
Ratios of Mean Changes and 95 CI
ITT PP 1 PP 2 Compl.
0.2
0.4
0.6
0.8
1
1.2
1.4
Lacidipine better
Atenolol better
8290 M
42
ESH/ESC vs JNC 7 - Major Agreements
Benefits of antihypertensive T Avoidance of
complex lab examinations BP measurement
procedure Use / value of ABPM / home BP Use of
antiplatelet / lipid lowering drugs BP targets
(and thresholds?) Follow-up strategies Value of
fixed / long-acting / low dose combinations Compe
lling drug indications (? more of format than of
substance) Combination T (as above) Treatment
of most specific conditions
6705 M
43
Progression of non-diabetic renal disease
A meta-analysis of data on 1860 pts on
antihypertensive regimens
Not including ACE-inhibitors
Including ACE-inhibitors
Blood Pressure
Urinary protein excretion
150
2.0
Systolic BP(mmHg)
1.8
140
1.6
139/85 vs 144/87 plt0.001
130
95
Urinary protein excretion g/d
1.4
90
Diastolic BP(mmHg)
1.2
85
plt0.001
80
1.0
Doubling of baseline serum creatinineconcentratio
n or ESD
Survival without end-stage renal disease
1.0
1.0
0.8
0.8
Survival without doubling of baseline serum
Creatinine concentration of ESRD
0.6
0.6
Survival without ESRD
0.4
0.4
0.2
0.2
plt0.001
plt0.003
0.0
0.0
0
12
24
36
48
0
12
24
36
48
Follow-up (mo)
Follow-up (mo)
Patient, n
919
752
632
404
63
Control
941
770
657
450
56
ACEI
Jafar TH, Ann Int Med 200113573-87.
44
Results of IDNT Primary Objective
Blood Pressure Irbesartan 140/77 Amlodipine 141/7
7 Placebo 144/80
RR 0.77 1.07 0.71
p-value 0.011 ns 0.001
irbesartan vs placebo amlodipine vs
placebo irbesartan vs amlodipine
ASH 2001
2283
45
Effect of Antihypertensive Treatment (n 10)
MAP (mmHg)
Start of treatment
GFR (ml/min/1.73 m2)
Albuminuria (?g/min)
Parving et al., Lancet 1983
4826 M
46
Stroke ACEI vs D/BB CA vs
D/BB ACEI vs CA CHD ACEI vs
D/BB CA vs D/BB ACEI vs
CA Heart failure ACEI vs D/BB CA
vs D/BB ACEI vs CA Major CV events
ACEI vs D/BB CA vs D/BB ACEI
vs CA CV death ACEI vs D/BB CA
vs D/BB ACEI vs CA Total mortality
ACEI vs D/BB CA vs D/BB ACEI
vs CA
Mean BP ? (mmHg) 2 / 0 0 / 0 1 /
1 2 / 0 0 / 0 1 / 1 2 / 0 0 /
0 1 / 1 2 / 0 0 / 0 1 / 1 2 /
0 0 / 0 1 / 1 2 / 0 0 / 0 1 / 1
Relative Risk (95 CI) 1.09 (1.00-1.18) 0.93
(0.86-1.01) 1.12 (1.01-1.25) 0.98
(0.91-1.05) 1.01 (0.94-1.08) 0.96
(0.88-1.05) 1.07 (0.96-1.19) 1.34
(1.22-1.47) 0.82 (0.73-0.92) 1.02
(0.98-1.07) 1.04 (0.99-1.08) 0.97
(0.92-1.03) 1.03 (0.95-1.11) 1.04
(0.97-1.12) 1.03 (0.94-1.13) 1.00
(0.95-1.05) 0.99 (0.94-1.04) 1.04 (0.98-1.10)
Favours first listed
Favours second listed
0.5
1.0
2.0
Relative risk
6396 M
47
Prevalence of Risk Factors in N (2446) and H
(2144) of the SMOOTH Study
Smoking
? BMI
? Ch
? TG
? HDL-Ch
? UA
DM
66.1
55.1
51.3
P lt 0.001
29.7
27.8
20.1
16.8
15.8
10.0
8.3
7.0
6.1
6.3
3.3
NS
7638 M
48
Intermediate Outcomes Biochemical Changes at 4
years
Potassium - mmol/L
4.1
Chlorthalidone
Plt.001
4.4
Amlodipine
Plt.001
4.5
Lisinopril
lt 3.5mmol/L
8.5
Chlorthalidone
Plt.001
1.9
Amlodipine
Plt.001
0.8
Lisinopril
5209 M
49
ALLHAT - K Supplementation Analysis
C 8
A 4
L 2
8081 M
50
Diuretic-Induced Hypokalemia
Common More lab examinations? ? Sudden
death? ? Protection by antihypertensive
treatment?
8097 M
51
Hazard Ratio of CVD According to Serum K of
Treated Patients at 1 Year in SHEP
1.18 (0.73-1.76)
K lt 3.5 mEq/l K 3.5 mEq/l
CVD CHD Stroke
0.61 (0.50-0.75)
1.46 (0.79-2.67)
0.75 (0.56-1.01)
1.43 (0.74-2.74)
0.51 (0.36-0,71)
0.1
0.5
1
2
5
10
Placebo better
Treatment better
4851
52
ESH/ESC Guidelines - Choice of Antihypertensive
Drugs
Choice influenced by - Previous patients
experience - Cost (to individual / health
provider) - Risk profile / TOD - CVD / Renal
disease - Diabetes - Coexisting disorders /
Drugs interactions - Patients
preference Emphasis on 1st choice drugs outdated
(predominance of combination T) Cost
consideration should not predominate over
efficacy / tolerability in any individual patients
6407 M
53
Dysmetabolic Effect of Diuretics ( BB)
? CVD / Nephropathy / ESRF More med. visits /
lab examinations More patients under
antidiabetic drugs More antihypertensive drugs
(lower BP targets) More antihypertensive drugs
in diabetics
8096 M
54
Changes in OGT Test (2h) after 12 Months
Antihypertensive T in ALPINE (n 49)
S-Insulin
P-glucose
S-Ins / P-Gluc
Candesartan, 16 mg
HCTZ, 25 mg
p lt 0.001 p 0.006
Lindholm et al., J Hypertens 2003 21 1563
8272 M
55
Biochemical Results Fasting Glucose (mg/dL)
Lisinopril
Amlodipine
Chlorthalidone
Total
Baseline
122.9 (56.1)
123.1 (57.0)
123.5 (58.3)
4 Years
121.5 (51.3)
123.7 (52.0)
126.3 (55.6)
Among baseline nondiabetics with baseline lt126
mg/dL
Baseline
93.3 (11.8)
93.0 (11.4)
93.1 (11.7)
100.5 (19.5)
103.1 (27.7)
104.4 (28.5)
4 Years
Diabetes Incidence (follow-up fasting glucose ?
126 mg/dL)
4 Years
8.1
9.8
11.6
plt.05 compared to chlorthalidone
5246 M
56
Systolic vs Diastolic BP Control in Trials on
Diabetic Hypertensives
120
200
mmHg
mmHg
SBP
DBP
Micro HOPE
190
CAPPP
110
INSIGHT
180
VALUE
HOT
100
170
UKPDS
STOP-2
160
90
FACET
150
LIFE
80
RENAAL
IDNT
140
IRMA
70
130
ABCD
B
T
B
T
120
60
Mancia G., Grassi G., J Hypertension 2002
1186 G
57
Cumulative Yearly Rates of Development of
Sight-Threatening Diabetic Retinopathy in 4770
Patients with Type 2 Diabetes
Cumulative incidence ()
p 0.0012 (for trend)
Patients at risk Level 30 Level 20 Level 10
217 810 3743
217 810 3743
175 732 3568
116 531 2558
69 355 1584
33 218 943
18 149 630
Younis N et al., Lancet 2003 361 195
7148 M
58
Prevalence () of Different Stages of Nephropathy
with Increasing Duration of Diabetes
Time (years) 0 5 10 15 20
Microalbuminuria or worse 7.3 17.3 24.9 28.0
34.3 (model)
Macroalbuminuria or worse 0.7 2.8 5.1
7.6 10.0 (model)
? SCr / renal replacement 0.0 0.4 0.8 2.3
Adler et al. - UKPDS, Kidney Int 2003 63 225
7156 M
59
RR of New Onset Diabetes in CAS (vs NCAS)
Patients in INVEST
7542 M
60
Cardiovascular Events in Hypertensive Subjects
with Regression versus Persistence or New
Development of Left Ventricular Hypertrophy
Study Muiesan (1995) Verdecchia
(1998) Cipriano (2001) Koren (2002) Total Het
erogeneity ?2 2.50 df 3 p 0.48 Z -2.71
p 0.0068
LVH regression 4/ 32 3/ 52 5/ 52
1/ 16 13/152
LVH persistence/new 15/ 41 13/100 17/134 12/
42 57/317
Odds Ratio (95 CI) 0.24 (0.07-0.84) 0.41
(0.11-1.51) 0.73 (0.25-2.10) 0.17
(0.02-1.40) 0.41 (0.21-0.78)
Odds Ratio (95 CI)
0.1
0.2
0.5
1
2
5
n 1064 FU 2.8-10.0 ys LVH at B 22
Favours LVH regression
Favours LVH persistence/new
LVH detected by echocardiography
Verdecchia P et al., Am J Hypertens 2003 16 895
8010 M
61
Low-Dose Diuretics as 1st Choice - 1993 WHO/ISH
Statement
It is contradictory to emphasize the need for
treatment to address global CV risk and
recommend as 1st choice treatments that may
increase it.
8094 M
62
Goal(s) of Treatment
In young / middle age / not high risk patients
treatment goal is not to prevent an (unlikely)
event in few years but to prevent progression (or
achieve regression) of silent organ damage that
will cause an event many years later.
7998 M
63
Superior Effect of New vs Conventional Drugs on
Markers of TOD (Intermediate End-Points)
LV hypertrophy Carotid artery IMT /
Atherosclerosis Arteriolar remodelling Urinary
protein excretion Endothelial dysfunction Arterial
stiffening Mild renal damage CA coronary content
ACEI / CA / ARB CA / ACEI ACEI / ARB / CA ACEI /
ARB CA / ACEI (?) / ARB (?) ? CA CA
6073 M
64
JNC7 vs ESH-ESC GLsMajor Differences
- Total CV risk assesment
- Term pre-hypertension avoided / no therapeutic
reccomendations if risk not high - Drug administration in grade I hypertension more
flexible - 5 drug classes (not only D) for T initiation /
maintenance - Intermediate end-points considered for risk
assessment / treatment goals - All trial (not only ALLHAT) considered
- Combination T as first choice
- Mention of ?-blockers / central agents
- Wider disclosure of conflict of interest
65
Definitions and classification of blood pressure
levels
Systolic (mmHg)
Diastolic (mmHg)
Category
Optimal lt120 lt80 Normal 120-129 80-84 High
normal 130-139 85-89 Grade 1 hypertension (mild)
140-159 90-99 Grade 2 hypertension
(moderate) 160-179 100-109 Grade 3 hypertension
(severe) ? 180 ? 110 Isolated systolic
hypertension ? 140 lt90
ESH/ESC 2003
66
2003 European Society of HypertensionEuropean
Society of Cardiology guidelines for the
management of arterial hypertension
Due to the importance of target organ damage in
determining the overall cardiovascular risk of
the hypertensive patient, evidence of organ
involvement should be sought carefully
the importance of organ damage, not only in
diagnosing cardiovascular risk but also in the
follow-up of patients, as well as in using
additional enpoints for assessing treatment
outcomes
Journal of Hypertension 2003
67
Unplanned Cross-Over Treatment in ALLHAT
C 13.2 9.0 22.2
A 16.6 6.9 23.5
L 15.7 8.5 24.2
Addition of comparison drug(s) Only taking
comparison drug(s) Total drug(s) classes
4856
68
RR of New Onset Diabetes in NCAS (vs CAS)
Patients in INVEST
7543 M
69
In ALPINE study risk of developing metabolic
syndrome 13 times greater with HCTZ (and BB) than
with ARB (and CA)
Lindholm et al., J Hypertension 2003 21 1563
7479 M
70
BP Range Termed Hypertension is Clinically
Heterogeneous
Very high CV risk High CV risk Moderate CV
risk Low CV risk
Drug treatment Drug treatment if BP high
normal Life style changes advisable No
intervention necessary (particularly if BP
normal)
7390 M
71
10 Year Risk of Fatal CVD in High Risk Regions of
Europe by Gender, Age, SBP, Total Cholesterol
and Smoking Status
6614 M
72
Are JNC-7 Recommendations Less Costly than
ESH/ESC Recommendations?
ESH/ESC More liberal recommendations, but those
patients in whom careful search has excluded TOD
more likely to have deferred treatment In
individuals with BP 120-139 or 80-89 mmHg only
if other risk factors or TOD are present In
individuals with BP gt 140 or 90 mmHg and no
additional risk factor only after up to 1 year
of lifestyle measures, and only if preferred by
the patients and resources available All major
classes of agents, but many patients with grade I
hypertension and low additional risk will not
necessarily receive drug treatment
JNC-7 Very simple, with poor characterization
of TOD In all individuals with BP 120-139 or
80-89 mmHg independently of other risk factors
and TOD In all individuals with BP gt 140 or 90
mmHg Thiazide diuretics for all individuals
with BP gt 140 or 90 mmHg without compelling
indications
Diagnostic Procedures Life-style Measures I
nitiation of Drug Treatment Drugs
7622 M
73
Death is in all living creatures future Should
they be called predeath?
7391 M
74
Relationship of CV Events and Organ Damage
Events do not take place on the background of a
healthy cardiovascular system but on the top of
subclinical organ damage
2936
75
High / Very High Risk Patients
BP gt 180/110 mmHg BP gt 130/ 85 mmHg if - Risk
factors gt 3 - Diabetes - Associated CVD - TOD
LVH CA thickening Microalbuminuria Mild renal
damage
Arterial remodelling? Endothelial
dysfunction? Arterial stiffening? Calcium
deposition?
6707 M
76
Arguments Opposing Diuretics (D) as Sole 1st
Choice in HT
No evidence that D more protective than other
drug classes No evidence from trials on D at low
dose BP lowering effect limited with D at low
doses Diabetogenic / dismetabolic effects of D
substantial Hypokalemic effect of D substantial
6447 M
77
CA vs D or BB (n 11685)
CVD
CV death
Stroke
CHD
CHF
Total mortality
14
12
4
1
1
? RR
statistically significant borderline
significant
-14
n events
1078
409
454
561
274
776
Coll Group, Lancet 2003
7775 M
78
ESH/ESC Guidelines Stratification of Risk to
Quantify Prognosis
Blood Pressure (mmHg)
Grade 1 SBP 140-159 or DBP 90-99
Grade 2 SBP 160-179 or DBP 100-109
Grade 3 SBP 180 or DBP 110
Normal SBP 120-129 or DBP 80-84
High Normal SBP 130-139 or DBP 85-89
Other Risk Factors and Disease History No other
risk factors 1-2 risk factors ACC
High added risk
Moderate added risk
Low added risk
Average risk
Average risk
Very high added risk
Moderate added risk
Moderate added risk
Low added risk
Low added risk
Very high added risk
High added risk
High added risk
High added risk
Moderate added risk
3 or more risk factors or TOD or diabetes
Very high added risk
Very high added risk
Very high added risk
Very high added risk
High added risk
ACC associated clinical conditions TOD target
organ damage SBP systolic blood pressure DBP
diastolic blood pressure
6252 M