Small Mission Hospital in Uganda PowerPoint PPT Presentation
1 / 52
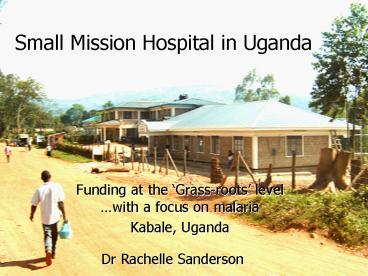
Title: Small Mission Hospital in Uganda
1
Small Mission Hospital in Uganda
- Funding at the Grass-roots level with a focus
on malaria - Kabale, Uganda
Dr Rachelle Sanderson
2
Summary
- Introduction
- 1. Funding infrastructure
- 2. Funding recurrent costs
- - malaria epidemic
- - insurance scheme
- 3. Funding specific projects
- Access to Project funding
- Conclusion
Uganda
3
Kabale, South West Uganda
- Population of 38,000
- No malaria before 1960, due to high altitude and
climate - Now malaria endemic
4
Kabale District
- Average monthly income 15
- Do not have savings so any costs in excess of
about 15 would often be met by selling capital
5
My role in the Project
- Church Missionary Society
- 2000-2005
- Medical Superintendent
- Financial Controller,
- under Management
- Committee, with
- external auditors.
6
Rugarama Health Centre
- Infrastructure necessary to run malaria programme
7
2000 46 inpatient beds
8
Funding Infrastructure
- Grants awarded in 2000/01
- Truro Episcopal Church, Virginia, USA
- Lions Clubs
- International,
- Sight First
- Campaign
9
November 2000 land cleared
10
June 2002 local fundraising
11
Community involvement enabling ownership
12
Open to the public Sept 2002
13
Opening of Children and Maternity unit in
December 2003
14
Staff Accommodation Unit
15
May 2004 accommodation complete
16
Needed Dental and Xray Block
17
June 2005 Unit completed
18
Funding infrastructure
- All capital costs from Outside organisations
- Christoffel Blinden Mission
- Lions Clubs International
- Trusts
- Missionary Organisations
- Churches
- Well wishers/supporters
19
Funding infrastructure
- Transparent and timely accountability
- Low costs mostly within or under budget
- Minimal sideway movement of money
- Tight schedule
- Approaching donors before use money in different
way to primary request - Impact on society
20
20,000 people made use of services of Rugarama
Health Centre in 2004/05
21
Funding recurrent costs
- 75-83 User fees, including Private patients
- Working towards sustainability
- However reduced accessibility to the poor, even
with Good Samaritan Fund and innovative ways of
helping those who cannot pay.
22
Funding recurrent costs
- 5 income from Government grant
- Remaining costs covered by donations and some
small income generating projects
23
Funding recurrent costs
- Expenditure kept low mainly by keeping salaries
low (trying to keep perks high) - But low morale
- high staff turn-over
24
Funding recurrent costs
- 5 Government Grant for Primary Health Care
- Negotiated to gain (mini) Hospital Status (Health
Centre IV), awarded in November 2004, put into
effect July 2005. - Grant up to 50 budget.
- Enabled salaries to (nearly) come in line with
Government equivalents
25
Malaria Epidemic
- November 2000 February 2001
- RHC 46 beds at 200 bed capacity
- (Normal capacity between 20 60)
26
Effects on Hospital
- Staffing levels
- Staff with malaria
- Medicine supply
- Equipment
- Space/capacity
27
Effects of Patients of getting malaria
- Various options
- 1. Be treated when first get sick.
- Cost
- Chloroquine/Fansidar - 2.00
- But resistance, so malaria returns
- Quinine/Fansidar - 4.25
- But unpleasant treatment for 1 week.
- Artenam/Fansidar - 7.00
28
Patient Options
- 2. Wait to see if will get better
- Get better probably did not have malaria
- Get worse do have malaria
29
Now need Hospital admissionCost minimum 10
(per person)Risk of sequelae or death
30
Patient Options
- 3. Avoid getting malaria Buy Mosquito net
- Cost 4.50
31
Insurance Scheme
- Set up in 2003
- Dairy Farmers Cooperative
- Funding from USAID via NGO Health Partners
- Started with 200 families of 4 or more members.
32
Insurance scheme
- Quarterly pre-payment
- Paid 0.5 per visit
- Included general health check, dental checks and
treatment, eye check up - Health Promotion Workshop included malaria
training - Subsidised mosquito nets
33
Limited success?
- Cooperatives did not pay in time
- Employ extra personnel to run the scheme,
primarily to chase payments - Extra staff to keep Cooperative members motivated
and educated - Whilst keeping costs down, who pays for the extra
staff?
34
Insurance scheme
- The Clients, when using the services, wanted
Private Style care - And yet wanted subsidised services
- Culture not familiar with
- insurance concept
- Culture not familiar with
- planning for the future
- When they did use the
- services, very pleased!
35
How to get people to change?
36
Funding of Specific Projects
- Sexy subjects - HIV/AIDS, Youth
Positive living Club
Post test Club for Adolescents
37
RHC Malaria Projects
- 1. Compassion International
- mosquito nets to their children
- training of volunteers to spray houses
- equipment and insecticide for spraying (only
their villages)
38
training of Community Health Workers in
diagnosing malaria and treating with CQ/fansidar
their villages
39
RHC Malaria Projects
- 2. Care International
- Training Volunteers in use of HOMEPAK
- 3. Poverty Alleviation Fund and others
- Free chloroquine and fansidar
40
4. Primary Health Care GrantVillage based
training about malaria
41
Occasional hitch.
42
RHC Malaria Projects
- 5. Church Donations
- Provision of mosquito nets for the Hospital
- During Hospital stay they would be taught how to
use nets - Subsidised nets to Pregnant women and to
malnourished children
43
Funding specific projects
- Lions Sight First Campaign
- Funding for 1 workshop per month over 3 years.
- sensitisation/mobilisation of the population
about eye service availability - Training of low level health workers in eye
- care issues
44
Lions Eye Training
- Successful sensitisation/mobilisation of the
population, using community leaders and local
health workers - Training has to be ongoing, not only to cover
whole District, but also to maintain awareness
over time
45
Access to Funding
- Dissemination of information about available
grants and how to apply for them was poor - Often find out about grants too late
- Right place at right time
46
Access to funding
- Global Fund application
- Not rewarded
- No feedback as to why
47
Access to funding
- Para-medical and administrative Staff lack
training - How to assess need
- How to write a Project Proposal
- How to implement the project
- How to be accountable to the donors
- Each new wave of workers needs training
48
Conclusions
- Disseminate information about grants to
grass-root level - Incorporate training in seeing projects through
from proposal writing through to accountability
49
Conclusions
- Subsidise prevention and control measures, to
make them affordable - Do by example! Get nets into Education and
Health Establishments
50
Conclusion
- Sensitise/mobilise community about malaria
prevention and control - Encourage early treatment Community Health
Workers, Homepak. - Educate, educate, educate population and health
workers over time, with aim to create cultural
shift
51
Summary
- Help those on the ground to do what they want to
do, to do more of what they are already doing, to
do it better, and to be able to offer it
subsidised or free to those who need it.
52
(No Transcript)