Journal Club PowerPoint PPT Presentation
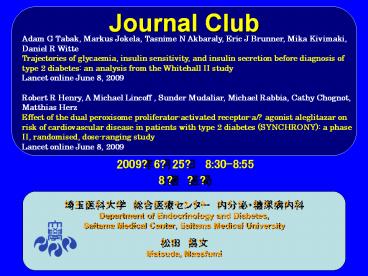
Title: Journal Club
1
Journal Club
Adam G Tabak, Markus Jokela, Tasnime N Akbaraly,
Eric J Brunner, Mika Kivimaki, Daniel R
Witte Trajectories of glycaemia, insulin
sensitivity, and insulin secretion before
diagnosis of type 2 diabetes an analysis from
the Whitehall II study Lancet online June 8,
2009 Robert R Henry, A Michael Lincoff , Sunder
Mudaliar, Michael Rabbia, Cathy Chognot, Matthias
Herz Effect of the dual peroxisome
proliferator-activated receptor-a/? agonist
aleglitazar on risk of cardiovascular disease in
patients with type 2 diabetes (SYNCHRONY) a
phase II, randomised, dose-ranging study Lancet
online June 8, 2009
2009?6?25? 830-855 8? ??
- ?????? ???????? ????????
- Department of Endocrinology and Diabetes,
- Saitama Medical Center, Saitama Medical
University - ?? ??
- Matsuda, Masafumi
2
(No Transcript)
3
Department of Epidemiology and Public Health,
University College London, London, UK (A G Tabak
MD, M Jokela PhD, T N Akbaraly PhD, E J Brunner
PhD, Prof M Kivimaki PhD, D R Witte MD)
Semmelweis University Faculty of Medicine, 1st
Department of Medicine, Budapest, Hungary (A G
Tabak) Department of Psychology, University of
Helsinki, Helsinki, Finland (M Jokela) INSERM
U888 and University Montpellier 1, Montpellier,
France (T N Akbaraly) Finnish Institute of
Occupational Health, Helsinki, Finland (Prof M
Kivimaki) and Steno Diabetes Center, Gentofte,
Denmark (D R Witte)
www.thelancet.com Published online June 8, 2009
4
All 3555-year-old non-industrial British civil
servants working in London offices (UK) of 20
departments were invited to participate in this
study.
10 308 (6895 men) were recruited between August,
1985, and April, 1988 (phase 1).26 Between
August, 1991, and December, 1994 (phase 3), all
participants known to be alive and in the country
were invited to the screening clinic for an oral
glucose tolerance test, and 6058 men and 2758
women (855 of the original sample) attended.
5
Background
Little is known about the timing of changes in
glucose metabolism before occurrence of type 2
diabetes. We aimed to characterise trajectories
of fasting and postload glucose, insulin
sensitivity, and insulin secretion in individuals
who develop type 2 diabetes.
6
Methods
We analysed data from our prospective
occupational cohort study (Whitehall II study) of
6538 (71 male and 91 white) British civil
servants without diabetes mellitus at baseline.
During a median follow-up period of 97 years,
505 diabetes cases were diagnosed (491 on the
basis of oral glucose tolerance test). We
assessed retrospective trajectories of fasting
and 2-h postload glucose, homoeostasis model
assessment (HOMA) insulin sensitivity, and HOMA
ß-cell function from up to 13 years before
diabetes diagnosis (diabetic group) or at the end
of follow-up (non-diabetics).
7
- 94
- 97
- mg/dl
10.2 6.5 65.9 36.1 microU/ml
8
126mg/dl
108mg/dl
Figure 1 Fasting (A) and 2-h postload (B)
glucose trajectories before diagnosis of diabetes
or the end of follow-up Numbers are 505 incident
diabetes cases and 6033 non-diabetics. Time 0 is
diagnosis for incident diabetes cases or end of
follow-up for non-diabetics. Multilevel
longitudinal modelling was done using linear
growth model for non-diabetic and piecewise
approach, including cubic terms for time, for
incident diabetic individuals with oral glucose
tolerance test fasting glucose (A) and 2-h
glucose (B) as outcomes. Analysis was adjusted
for age, sex, ethnic origin, and study phase.
Estimations were done for a hypothetical
population consisting of 71 male, 91 white
individuals aged 63 years at time 0 years. Error
bars show 95 CI for the fixed effects. Tables
show the number of measurements for each year at
and before diabetes diagnosis or the end of
follow-up.
9
198mg/dl
Figure 1 Fasting (A) and 2-h postload (B)
glucose trajectories before diagnosis of diabetes
or the end of follow-up Numbers are 505 incident
diabetes cases and 6033 non-diabetics. Time 0 is
diagnosis for incident diabetes cases or end of
follow-up for non-diabetics. Multilevel
longitudinal modelling was done using linear
growth model for non-diabetic and piecewise
approach, including cubic terms for time, for
incident diabetic individuals with oral glucose
tolerance test fasting glucose (A) and 2-h
glucose (B) as outcomes. Analysis was adjusted
for age, sex, ethnic origin, and study phase.
Estimations were done for a hypothetical
population consisting of 71 male, 91 white
individuals aged 63 years at time 0 years. Error
bars show 95 CI for the fixed effects. Tables
show the number of measurements for each year at
and before diabetes diagnosis or the end of
follow-up.
10
(No Transcript)
11
Figure 2 Homoeostasis model assessment (HOMA)
insulin sensitivity (A) and HOMA ß-cell function
trajectories (B) before diagnosis of diabetes or
the end of follow-up Numbers are 505 incident
diabetes cases and 6033 non-diabetics. Time 0 is
diagnosis for incident diabetes cases or end of
follow-up for non-diabetics. Multilevel
longitudinal modelling was done using linear
growth model for non-diabetic and non-piecewise
or piecewise approach, including linear or
quadratic terms for time, for incident diabetic
individuals with HOMA2-S (A) and HOMA2-B (B) as
outcomes. Analysis was adjusted for age, sex,
ethnic origin, and study phase. Estimations were
done for a hypothetical population consisting of
71 male, 91 white individuals aged 63 years at
time 0 years. Error bars show 95 CI for the
fixed effects. Tables show the number of
measurements for each year at and before diabetes
diagnosis or the end of follow-up.
HOMA2-Shomoeostasis model assessment insulin
sensitivity. HOMA2-Bhomoeostasis model
assessment ß-cell function.
12
Figure 2 Homoeostasis model assessment (HOMA)
insulin sensitivity (A) and HOMA ß-cell function
trajectories (B) before diagnosis of diabetes or
the end of follow-up Numbers are 505 incident
diabetes cases and 6033 non-diabetics. Time 0 is
diagnosis for incident diabetes cases or end of
follow-up for non-diabetics. Multilevel
longitudinal modelling was done using linear
growth model for non-diabetic and non-piecewise
or piecewise approach, including linear or
quadratic terms for time, for incident diabetic
individuals with HOMA2-S (A) and HOMA2-B (B) as
outcomes. Analysis was adjusted for age, sex,
ethnic origin, and study phase. Estimations were
done for a hypothetical population consisting of
71 male, 91 white individuals aged 63 years at
time 0 years. Error bars show 95 CI for the
fixed effects. Tables show the number of
measurements for each year at and before diabetes
diagnosis or the end of follow-up.
HOMA2-Shomoeostasis model assessment insulin
sensitivity. HOMA2-Bhomoeostasis model
assessment ß-cell function.
13
Results
Multilevel models adjusted for age, sex, and
ethnic origin confirmed that all metabolic
measures followed linear trends in the group of
non-diabetics (10 989 measurements), except for
insulin secretion that did not change during
follow-up. In the diabetic group (801
measurements), a linear increase in fasting
glucose was followed by a steep quadratic
increase (from 579 mmol/L to 740 mmol/L)
starting 3 years before diagnosis of diabetes.
2-h postload glucose showed a rapid increase
starting 3 years before diagnosis (from 760
mmol/L to 1190 mmol/L), and HOMA insulin
sensitivity decreased steeply during the 5 years
before diagnosis (to 867). HOMA ß-cell function
increased between years 4 and 3 before diagnosis
(from 850 to 926) and then decreased until
diagnosis (to 624).
14
Conclusion
In this study, we show changes in glucose
concentrations, insulin sensitivity, and insulin
secretion as much as 36 years before diagnosis
of diabetes. The description of biomarker
trajectories leading to diabetes diagnosis could
contribute to more-accurate risk prediction
models that use repeated measures available for
patients through regular check-ups. Funding
Medical Research Council (UK) Economic and
Social Research Council (UK) British Heart
Foundation (UK) Health and Safety Executive
(UK) Department of Health (UK) National
Institute of Health (USA) Agency for Health Care
Policy Research (USA) the John D and Catherine T
MacArthur Foundation (USA) and Academy of
Finland (Finland).
15
(No Transcript)
16
Department of Medicine, University of California
at San Diego and VA San Diego Healthcare System,
San Diego, CA, USA (Prof R R Henry MD, S Mudaliar
MD) Department of Cardiovascular Medicine,
Cleveland Clinic, Cleveland, OH, USA (Prof A M
Lincoff MD) Hoff mann-La Roche, Nutley, NJ, USA
(M Rabbia MA) and F Hoff mann-La Roche AG,
Basel, Switzerland (C Chognot PhD, M Herz MD)
www.thelancet.com Published online June 8, 2009
17
Figure Synergistic beneficial actions of
balanced PPAR-a/? agonists Apo
AIapolipoprotein A1. Apo AIIapolipoprotein A2.
Apo CIIIapolipoprotein C3. FAfatty acids.
FFAfree fatty acids. Figure adapted from
Balakumar and colleagues and Fievet and colleagues
18
Aleglitazar is a peroxisome proliferator-activated
receptor agonist (hence a PPAR modulator ) with
affinity to PPARa and PPAR?,
This class includes muraglitazar and
tesaglitazar. Both were discontinued owing to
safety concerns, including increase in serum
creatinine and decrease in glomerular filtration
rate (tesaglitazar) or increased risk of
cardiovascular events (muraglitazar).
19
BACKGROUND
Despite previous reports of potential adverse
cardiovascular effects of peroxisome
proliferator-activated receptor (PPAR) agonists,
the promise for PPAR agonists to positively
affect risk of cardiovascular disease in patients
with type 2 diabetes is of continued interest.
The SYNCHRONY study aimed to establish the
glucose-lowering and lipid-modifying effects, and
safety profile, of the dual PPAR-a and PPAR-?
agonist aleglitazar.
20
METHODS
In this double-blind study, patients with type 2
diabetes (either drug-naive or pre-treated with
two oral agents) were enrolled from 47 sites in
seven countries. After a single-blind, 45-week
placebo run-in period, 332 patients were
randomised double-blind (via an interactive
voice-response system) to 16 weeks treatment
with aleglitazar at once-daily doses of 50 µg,
150 µg, 300 µg, or 600 µg, or matching placebo
(n55 in each group), or to open-label
pioglitazone 45 mg once daily (n57) as a
reference. The primary efficacy endpoint was the
change in glycosylated haemoglobin (HbA1c)
concentration from baseline to the end of
treatment. Patients who received at least one
dose of study drug and had at least one evaluable
post-baseline HbA1c measurement were included in
the efficacy analysis. This study is registered
with ClinicalTrials.gov, number NCT00388518.
21
Figure 1 Trial profile
22
Table 1 Baseline (after placebo run-in period)
demographic and clinical characteristics (safety
population)
23
Figure 2 Effect on haemoglobin A1c concentration
(A) Absolute change from baseline to end of
treatment period (week 16) and (B) over time.
Analysis undertaken in the intention-to-treat
population, LOCF. p values are versus placebo.
LSleast squares. HbA1chaemoglobin A1c.
24
Figure 2 Effect on haemoglobin A1c concentration
(A) Absolute change from baseline to end of
treatment period (week 16) and (B) over time.
Analysis undertaken in the intention-to-treat
population, LOCF. p values are versus placebo.
LSleast squares. HbA1chaemoglobin A1c.
25
Figure 3 Effect on fasting plasma glucose (A)
Absolute change from baseline to end of treatment
period (week 16) and (B) over time. Analysis
undertaken in the intention-to-treat population,
LOCF. p values are versus placebo. LSleast
squares. FPGfasting plasma glucose.
26
Figure 3 Effect on fasting plasma glucose (A)
Absolute change from baseline to end of treatment
period (week 16) and (B) over time. Analysis
undertaken in the intention-to-treat population,
LOCF. p values are versus placebo. LSleast
squares. FPGfasting plasma glucose.
27
Figure 4 Eff ect on lipid parameters Percentage
change from baseline lipid concentrations to end
of treatment period (week 16) for (A)
triglycerides, (B) HDL cholesterol, (C) LDL
cholesterol, and (D) apolipoprotein B. Analysis
undertaken in the intention-to-treat population,
LOCF. p values are versus placebo. LSleast
squares.
28
(No Transcript)
29
(No Transcript)
30
RESULTS
The efficacy analysis excluded six patients (n0
in pioglitazone group n1 in each of placebo, 50
µg, 150 µg, and 600 µg aleglitazar groups and
n2 in 300 µg aleglitazar group). Aleglitazar
significantly reduced baseline HbA1c versus
placebo in a dose-dependent manner, from 036
(95 CI 000 to 070, p0048) with 50 µg to
135 (099 to 170, plt00001) with 600 µg.
The trend of changes over time suggests that the
maximum effect of aleglitazar on HbA1c
concentration was not yet reached after 16 weeks
of treatment. Oedema, haemodilution, and weight
gain occurred in a dose-dependent manner.
However, at aleglitazar doses less than 300 µg,
no patients had congestive heart failure,
frequency of oedema was similar to placebo (one
case at 50 µg, two at 150 µg, and three with
placebo) and less than with pioglitazone (four
cases), and bodyweight gain was less than with
pioglitazone (052 kg at 150 µg vs 106 kg).
31
CONCLUSION
The favourable balance in the safety and efficacy
profile of aleglitazar represents encouraging
short-term clinical data for this agent and
provides good evidence to enter phase III
investigation. Funding F Hoff mann-La Roche
AG (Switzerland).
32
(No Transcript)