Journal Club - PowerPoint PPT Presentation
Title:
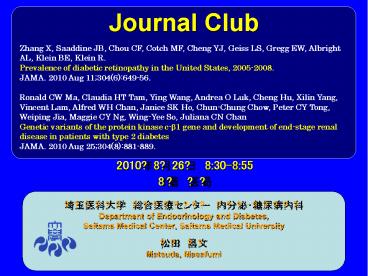
Journal Club
Description:
Journal Club Zhang X, Saaddine JB, Chou CF, Cotch MF, Cheng YJ, Geiss LS, Gregg EW, Albright AL, Klein BE, Klein R. Prevalence of diabetic retinopathy in the United ... – PowerPoint PPT presentation
Number of Views:407
Avg rating:3.0/5.0
Title: Journal Club
1
Journal Club
Zhang X, Saaddine JB, Chou CF, Cotch MF, Cheng
YJ, Geiss LS, Gregg EW, Albright AL, Klein BE,
Klein R. Prevalence of diabetic retinopathy in
the United States, 2005-2008. JAMA. 2010 Aug
11304(6)649-56. Ronald CW Ma, Claudia HT Tam,
Ying Wang, Andrea O Luk, Cheng Hu, Xilin Yang,
Vincent Lam, Alfred WH Chan, Janice SK Ho,
Chun-Chung Chow, Peter CY Tong, Weiping Jia,
Maggie CY Ng, Wing-Yee So, Juliana CN
Chan Genetic variants of the protein kinase c-b1
gene and development of end-stage renal disease
in patients with type 2 diabetes JAMA. 2010 Aug
25304(8)881-889.
2010?8?26? 830-855 8? ??
- ?????? ???????? ????????
- Department of Endocrinology and Diabetes,
- Saitama Medical Center, Saitama Medical
University - ?? ??
- Matsuda, Masafumi
2
(No Transcript)
3
Division of Diabetes Translation, National Center
for Chronic Disease Prevention and Health
Promotion, Centers for Disease Control and
Prevention, Atlanta, Georgia (Drs Zhang,
Saaddine, Chou, Cheng, Geiss, Gregg, and
Albright) Division of Epidemiology and Clinical
Applications, National Eye Institute, National
Institutes of Health, Bethesda, MD (Dr Cotch)
Department of Ophthalmology and Visual Sciences,
University of Wisconsin, School of Medicine and
Public Health, Madison, Wisconsin (Drs B. Klein
and R. Klein)
JAMA. 2010304(6)649-656
4
DIABETIC RETINOPATHY IS THE leading cause of new
cases of legal blindness among adults aged 20 to
74 years in the United States. Klein R, Klein B.
Vision disorders in diabetes. In National
Diabetes Data Group, ed. Diabetes in America. 2nd
ed. Bethesda, MD National Institutes of Health,
National Institute of Diabetes and Digestive and
Kidney Diseases 1995293337.
1988-1994 (National Health and Nutrition
Examination Surveys III NHANES III).
5
Background
Context The prevalence of diabetes in the United
States has increased. People with diabetes are at
risk for diabetic retinopathy. No recent national
population-based estimate of the prevalence and
severity of diabetic retinopathy exists.
Objectives To describe the prevalence and risk
factors of diabetic retinopathy among US adults
with diabetes aged 40 years and older.
6
Methods
Design, Setting, and Participants Analysis of a
cross-sectional, nationally representative sample
of the National Health and Nutrition Examination
Survey 2005-2008 (N1006). Diabetes was defined
as a self-report of a previous diagnosis of the
disease (excluding gestational diabetes mellitus)
or glycated hemoglobin A1c of 6.5 or greater.
Two fundus photographs were taken of each eye
with a digital nonmydriatic camera and were
graded using the Airlie House classification
scheme and the Early Treatment Diabetic
Retinopathy Study severity scale. Prevalence
estimates were weighted to represent the
civilian, non institutionalized US population
aged 40 years and older. Main Outcome
Measurements Diabetic retinopathy and
vision-threatening diabetic retinopathy.
7
Vision-threatening diabetic retinopathy, a level
that may soon result in vision loss if left
untreated, was defined as the presence of severe
non proliferative diabetic retinopathy,
proliferative diabetic retinopathy, or clinically
significant macular edema.
8
(No Transcript)
9
(No Transcript)
10
(No Transcript)
11
Results
Results The estimated prevalence of diabetic
retinopathy and vision-threatening diabetic
retinopathy was 28.5 (95 confidence interval
CI, 24.9-32.5) and 4.4 (95 CI, 3.5-5.7)
among US adults with diabetes, respectively.
Diabetic retinopathy was slightly more prevalent
among men than women with diabetes (31.6 95
CI, 26.8-36.8 vs 25.7 95 CI, 21.7-30.1
P.04). Non- Hispanic black individuals had a
higher crude prevalence than non-Hispanic white
individuals of diabetic retinopathy (38.8 95
CI, 31.9-46.1 vs 26.4 95 CI, 21.4-32.2
P.01) and vision-threatening diabetic
retinopathy (9.3 95 CI, 5.9-14.4 vs 3.2
95 CI, 2.0-5.1 P.01). Male sex was
independently associated with the presence of
diabetic retinopathy (odds ratio OR, 2.07 95
CI, 1.39-3.10), as well as higher hemoglobin A1c
level (OR, 1.45 95 CI, 1.20- 1.75), longer
duration of diabetes (OR, 1.06 per year duration
95 CI, 1.03-1.10), insulin use (OR, 3.23 95
CI, 1.99-5.26), and higher systolic blood
pressure (OR, 1.03 per mm Hg 95 CI, 1.02-1.03).
12
Conclusion
Conclusion In a nationally representative sample
of US adults with diabetes aged 40 years and
older, the prevalence of diabetic retinopathy and
vision-threatening diabetic retinopathy was high,
especially among Non-Hispanic black individuals.
13
Message/Comments
???????????????????????????????????? ????????????
???????????45??????????????????????????????
14
(No Transcript)
15
Activation of PKC in diabetic kidney by
hyperglycemia leading to multiple pathological
changes in diabetic nephropathy
Ruboxistaurin LY 333531
Fundamental Clinical Pharmacology 22 (2008)
231240
16
Protein kinase C, beta 1
LY333531 administration in diabetic rats resulted
in near normalization of GFR and filtration
fraction. Use of PKC b inhibitor in a small
patient population of type 2 DN showed a
significant reduction in albuminuria, prevented
loss of eGFR and improvement in renal function
A new drug application seeking approval from
USA-FDA for ruboxistaurin for the treatment of
moderate to severe non-proliferative diabetic
retinopathy was submitted by Eli Lilly in
February 2006. Lilly received an approval letter
from the FDA in August, 2006. FDA requested
additional 3-year, phase 3 clinical trial to
provide additional efficacy data before approving
the drug in moderate to severe non-proliferative
retinopathy. 17 April 2007 The manufacturer of
ruboxistaurin has advised us that they have
withdrawn regulatory applications in relation to
this product at this time. The Institute has
therefore decided to remove this appraisal from
its work programme.
17
Department of Medicine and Therapeutics (Drs Ma,
Wang, Luk, Yang, Chow, Tong, Ng, So, and J. Chan
Mss Tam and Ho and Messrs Lam and A. Chan), Hong
Kong Institute of Diabetes and Obesity (Drs Ma
and J. Chan), and Li Ka Shing Institute of Health
Sciences (Dr J. Chan), Chinese University of Hong
Kong, Prince of Wales Hospital, Shatin, New
Territories, Hong Kong SAR, China and Department
of Endocrinology and Metabolism, Shanghai
Clinical Center of Diabetes, Shanghai Jiaotong
University Affiliated Sixth Peoples Hospital,
Shanghai Diabetes Institute, Shanghai Key
Laboratory of Diabetes Mellitus, Shanghai, China
(Drs Hu and Jia). Dr Ng is now with Department of
Pediatrics, Section on Medical Genetics, Centers
for Diabetes Research and Human Genomics, Wake
Forest University School of Medicine,
Winston-Salem, North Carolina.
JAMA. 2010304(8)881-889
18
Background
Context Protein kinase C-ß (PKC-ß) is a
cell-signaling intermediate implicated in
development of diabetic complications.
Objective To examine the risk association of
PKC- ß1 gene (PRKCB1) polymorphisms and end-stage
renal disease (ESRD) in an 8-year prospective
cohort of Chinese patients with type 2 diabetes.
19
Methods
Design, Setting, and Participants We genotyped 18
common tag single nucleotide polymorphisms (SNPs)
that span the PRKCB1 gene (r20.80) in 1172
Chinese patients (recruited 1995-1998) without
renal disease at baseline. A validation cohort
included an additional 1049 patients with
early-onset diabetes who were free of renal
disease at baseline and were recruited after
1998. Main Outcome Measures Associations of
PRKCB1 polymorphisms under additive, dominant,
and recessive genetic models with new onset of
ESRD (defined as estimated glomerular filtration
ratelt15 mL/min/1.73m2 or dialysis or
renal-related death) were assessed by Cox
proportional hazard regression, adjusted for all
conventional risk factors including use of
medications
20
(No Transcript)
21
(No Transcript)
22
(No Transcript)
23
Adjusted for mean values of sex, age, duration of
diabetes, systolic and diastolic blood pressure,
hemoglobin A1c, total cholesterol, natural
logarithm of triglycerides, estimated glomerular
filtration rate, natural logarithm of albumin
excretion rate, retinopathy (present/absent),and
use of medications (yes/no). Three significant
and independent single-nucleotide polymorphisms
with r2lt0.80 (rs3760106 with the dominant model,
rs7404928 with the recessive model, and rs4787733
with the additive model) were selected to
calculate the number of risk alleles for
end-stage renal disease (ESRD).
24
(No Transcript)
25
Results
Results After a mean (SD) of 7.9 (1.9) years, 90
patients (7.7) progressed to ESRD. Four common
SNPs were associated with ESRD (Plt.05). The
closely linked T allele at rs3760106 and G allele
rs2575390 (r20.98) showed the strongest
association with ESRD (hazard ratio HR, 2.25
95 confidence interval CI, 1.31-3.87 P.003,
and HR, 2.26 95 CI, 1.31-3.88 P.003,
respectively). Four common variants predicted
ESRD in separate models. The HR for ESRD
increased with increasing number of risk alleles
(Plt.001) in the joint effect analysis. The
adjusted risk for ESRD was 6.04 (95 CI,
2.00-18.31) for patients with 4 risk alleles
compared with patients with 0 or 1 risk allele.
Incidence was 4.4 per 1000 person-years (95 CI,
0.5-8.2) among individuals with 0 or 1 risk
allele compared with 20.0 per 1000 person-years
(95 CI, 8.8-31.1) in those carrying 4 risk
alleles (6.9 of the cohort). These results were
validated in a separate prospective cohort of
young-onset diabetic patients. Of 1049 patients
in the validation cohort, 151 (14.3) developed
chronic kidney disease (CKD) during follow-up,
and there were significant associations between
both the T allele of rs3760106 and the G allele
of rs2575390 and development of CKD (HR, 1.68
95 CI, 1.10-2.57 P.02, and HR, 1.62 95 CI,
1.07-2.47 P.02, respectively).
26
Conclusion
Conclusion Genetic variants in the PRKCB1 gene
were independently associated with development of
ESRD in Chinese patients with type 2 diabetes.
27
Message
PKC-b1???????????????????????????? ??????????????
???????????????????????PKC-b1????????????????????
????????? Araki S, Haneda M, Sugimoto T, et al.
Polymorphisms of the protein kinase C-beta gene
(PRKCB1) accelerate kidney disease in type 2
diabetes without overt proteinuria. Diabetes
Care. 200629(4)864-868. T allele at 1054 C/T
and G allele at 546 C/G
28
(No Transcript)










![[PDF] Samurai Jack Hardcover Ruled Journal Ipad PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10094088.th0.jpg?_=20240808075)















![[PDF] Horror Movie Review Journal: Film Lovers Notebook for Reviewing 100 Movies, Cinema Journal, Pre Numbered Pages, A Film Review Log Book Full PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10089868.th0.jpg?_=202408010110)



